Advair Diskus
| Contato
Página Inicial

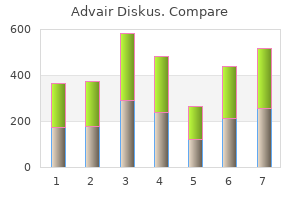
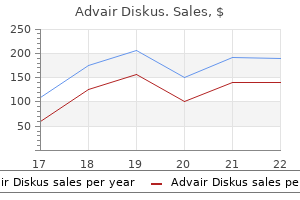
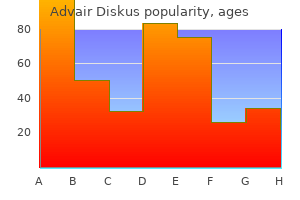
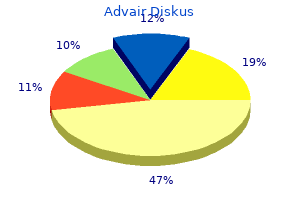
"Purchase advair diskus 250 mcg online, asthma vcd treatment".
J. Ali, M.B.A., M.B.B.S., M.H.S.
Medical Instructor, Creighton University School of Medicine
After disconnecting the cartilaginous septum from the bony septum by a quantity of vertical chondrotomies asthma levels cheap advair diskus 100 mcg on-line, its base should asthma symptoms phlegm advair diskus 250 mcg order otc be dissected and dislocated from the premaxilla and anterior nasal backbone to create a "swinging door" and supply wide entry to the posterior septum asthma forecast cheap 100 mcg advair diskus mastercard. Steps Steps the first vertical chondrotomy is made simply anterior to the primary fracture line asthma definition ziggurat advair diskus 500 mcg purchase online. A second vertical chondrotomy is made both at the second fracture line or on the cartilaginoussseous junction, relying on the deformity. A right-handed surgeon standing on the best side of the patient will generally choose to transfer the cartilaginous plate to the left. The cartilaginous septum has been mobilized and is dislocated to the left with a speculum to acquire wide access to the bony septum, vomer, and perpendicular plate. However, no cartilage is resected beneath the K space or from the septal base in the area of the anterior nasal spine. Resections in these areas may result in endorotation of the septal cartilage, which in flip will lead to postoperative sagging of the dorsum and retraction of the columella. A cartilaginous and bony crest may impede an try to dissect the septal base from the premaxilla and maxillary crest. Vertical Strips Vertical Strip on the Chondro-Osseous Junction A narrow, triangular, vertical strip could additionally be resected at the chondroperpendicular junction to facilitate mobilization of the cartilaginous septum. Horizontal Strips Horizontal Basal Strip A horizontal basal strip may be resected to get hold of greater mobility of the septal plate, facilitate its repositioning, and procure wide entry to the bony septum. Note the two areas the place no cartilage is resected to avoid endorotation of the septal plate. Horizontal Strip at a Horizontal Fracture A horizontal strip will normally have to be resected on the degree of a horizontal fracture to allow repositioning of the deviated parts. This too is finished in a conservative approach to avoid creating a gap that may lead to lack of assist of the dorsum. Bony and Cartilaginous Crest A bony and cartilaginous (basal) crest has usually to be eliminated. A horizontal chondrotomy is made simply above the crest, allowing the cartilaginous a half of the crest to be dissected and removed. If sure components still are likely to deviate, the mucoperichondrium and mucoperiosteum might need to be additional elevated. A resistant cartilaginous deviation could require an extra vertical or horizontal chondrotomy, or resection of a considerably bigger or further strip. Sometimes, the cartilaginous septum can solely be straightened by separating it from the triangular cartilages. One ought to never rely on "repositioning" the septum using strain of some kind of endonasal tamponade. Bony and Cartilaginous Deviation A bony and cartilaginous deviation is both resected or fractured into the midline with a strong forceps (Craig type). Resection is carried out by means of a forceps, bone scissors, or osteotome, relying on the deformity and the thickness of the bone. The resected area is later reconstructed by reimplanting plates of removed bone or cartilage. All faulty components of the septal skeleton are repaired by inserting plates of bone or cartilage. Rebuilding the septum serves numerous purposes: Maintaining and restoring the help and projection of the cartilaginous pyramid and lobule Restoring the traditional stiffness and thickness of the septum, thus preventing well-known sequelae of submucous resection, similar to late perforations, mucosal atrophy, and mucosal fluttering during respiration Facilitating revision surgical procedure Bony Spur A posterior bony spur can only be corrected by resection. A spur is dissected and mobilized utilizing an elevator and an osteotome, and eliminated with a forceps. Inserting small plates of bone and cartilage, made by slicing or slightly crushing resected components, subsequently suffices. It is a precondition of a good practical and aesthetic end result, and it can prevent problems corresponding to postoperative bleeding, hematomas, ecchymosis, and edema. Various methods could also be used, similar to inner dressings, special sutures, or internal and exterior splinting. The alternative depends upon the kind of surgery carried out and the non-public preference of the surgeon. A lengthy speculum is placed into the septal space, and remnants of blood are removed by suction to keep away from a septal hematoma. Small plates of bone (or cartilage, if inadequate bone is available) are inserted into the posterior septal space utilizing a protracted bayonet forceps. These small plates are made from the resected bony and cartilaginous septum, either by slicing or using a crusher. The pieces of bone and/or cartilage are placed mosaicfashion on the within of the left mucosal flap. The mucosal flaps are brought together by adjusting the interior dressings intranasally. Internal Dressings Internal dressings are used to maintain the reconstructed septum in the midline and stop a septal hematoma. They may serve to assist the nasal bones and cartilaginous pyramid in their new position. These dressings encompass a polyvinyl acetate sponge impregnated with oxidized cellulose. The septal area is closed by bringing the two mucosal flaps gently along with the interior dressings, using the blunt end of the elevator. A posterior septal defect is repaired by inserting plates of bone or cartilage with a long (14 cm) bayonet forceps (see Phase 5: Reconstruction). Many surgeons apply the internal dressings on the very finish of the operation, after closing all incisions. Others favor to apply the self-expanding internal dressings first, close the septal house, reconstruct the posterior septum, after which finally fixate the anterior septum in place and suture the varied incisions. The internal dressing is fixed to the nasal dorsum to stop it from slipping into the nasopharynx. Sutures and Splints Guide Sutures Guide sutures are used to maneuver the cartilaginous and bony plates into place. Just earlier than closing, a small minimize is made into the frenulum to bury the suture deep to the mucosa. Septospinal Suture If the septal base has the tendency to slip off the anterior nasal backbone and premaxilla, the septal plate could also be held in place by a septospinal suture. A slowly resorbable three suture is passed through the septal base, downward by way of the connective tissue fibers and the buccal mucosa on the left side of the anterior nasal backbone and the frenulum of the upper lip, after which again by way of the mucosa and the connective tissue on the best side of the nasal backbone. In reconstructing the septum, transseptal fixation sutures and septal splints could additionally be of great assist. It is lifted upward and exorotated until the cartilaginous dorsum has reached the specified level. Fixation of the Septal Base in a Groove within the Premaxilla To stabilize the septum, a groove may be cut in the course of the premaxilla with a 4-mm or 7-mm chisel. It results in respiration obstruction on inspiration and sometimes additionally to cosmetic complaints because of the visible protrusion of the caudal septal end into the nostril. A vertical chondrotomy is made on the bend (fracture line) on the other facet, and the septal base is disconnected from the anterior nasal spine and premaxilla. In circumstances with severe scarring, a unilateral or bilateral inferior tunnel may also be required (three-tunnel or four-tunnel approach). It solely stays connected to the posterior a half of the septum underneath the nasal dorsum. In spite of those resections, the anterior septum could are likely to return to its dislocated position. Fixation of the caudal septal finish by septocolumellar sutures and a septospinal suture. Such a graft is usually 20 to 25 mm long, considerably longer than the height of the still intact more posterior a half of the septum. If no septal cartilage is available, auricular cartilage is the second alternative (see page 244 and page 350). This graft corrects the retracted columella and the underprojected An incision (here, the time period hemitransfixion could be correct! A columellar pocket is created in the membranous septum using small, sharp and blunt curved scissors.
The quantity of aponeurosis masking the postcondylar groove asthma definition pdf 250 mcg advair diskus cheap with mastercard, in addition to the area between the 2 heads of the flexor carpi ulnaris asthma symptoms shaking order 250 mcg advair diskus mastercard, is variable asthma jobs order advair diskus 100 mcg line. In reality asthma 7 month old order advair diskus 250 mcg overnight delivery, some patients may not have this covering at all, allowing the ulnar nerve to slip, or "snap" over the medial epicondyle during forearm flexion. The anconeus epitrochlearis muscle is current in approximately 10% of the population. This muscle spans from the medial epicondyle to the olecranon and is a potential cause of ulnar nerve irritation. The ulnar nerve often supplies only one major branch to the flexor digitorum profundus, which arises after the branches destined for the flexor carpi ulnaris have already exited. The ulnar nerve passes immediately from the medial epicondyle to the pisiform bone in the wrist. In the distal third of the forearm, the ulnar nerve is not covered by muscle; it lies between the flexor carpi ulnaris tendon medially and the flexor digitorum superficialis tendon laterally. The ulnar artery, a branch of the brachial artery within the antecubital fossa, steadily makes its means medially to pair up with the ulnar nerve proximal to the wrist. Once together, these two buildings enter the hand, with the artery lateral to the nerve. Two sensory branches originate from the ulnar nerve within the distal half of the forearm. The first is the dorsal ulnar cutaneous nerve, which arises roughly 5 to 10 cm proximal to the wrist crease off the dorsomedial aspect of the ulnar nerve. This branch travels to the dorsum of the distal forearm between the ulna and the tendon of the flexor carpi ulnaris. Once on the dorsal surface, it pierces the antebrachial fascia and becomes subcutaneous a quantity of centimeters proximal to the wrist. The second sensory department from the ulnar nerve is the palmar ulnar cutaneous nerve, which is a mirror picture of the palmar cutaneous branch of the median nerve. The palmar ulnar cutaneous nerve branches from the volar-lateral floor of the ulnar nerve approximately 5 to 10 cm proximal to the wrist. It runs adherent to the ulnar nerve for a couple of centimeters then enters the subcutaneous area proximal to the distal wrist crease and arborizes over the hypothenar eminence. Although the dorsal ulnar cutaneous nerve often originates proximal to the palmar ulnar cutaneous nerve, in sure folks the reverse may be true. Alternatively, the dorsal ulnar cutaneous nerve may very well branch from the superficial sensory radial nerve. Communication, or cross discuss, between the ulnar nerve and the anterior interosseous nerve via the Martin-Gruber anastomosis may occur within the forearm (see Chapter 1, Median Nerve). There is another protuberance, now on the distal lateral aspect: the hook of the hamate. However, the superficial palmar carpal ligament is the lateral wall for the proximal portion of the tunnel only. The flexor carpi ulnaris tendon and the more distal pisiform bone (first bump within the wall described earlier) type the proximal, medial wall of the tunnel. In the distal half of the tunnel, the lateral wall is fashioned by the hook of the hamate (second bump within the wall described previously), whereas the shorter medial wall is formed by the pisiform bone. The distal ground is fashioned initially by the pisohamate ligament, then by the pisometacarpal ligament. However, a muscular arch from the pisiform bone to the hook of the hamate types the roof of the deeper, distal department tunnel. As their names indicate, the superficial department programs by way of the medial, more superficial tunnel with the ulnar artery, whereas the deep branch goes under the arch created by the flexor digiti minimi with a profunda or deep arterial department. Prior to this arch, the deep department of the ulnar nerve yields a small facet department that innervates the hypothenar muscles. The superficial branch splits into digital nerves destined for the fourth and fifth digits. Occasionally, there could also be early branching of the ulnar nerve with an anomalous course. For example, the ulnar nerve might branch proximal to the pisiform bone, with the superficial sensory branch communicating some, or all, of its sensory fibers to the palmar ulnar cutaneous nerve. A second variation occurs when the deep motor branch bifurcates previous to entering the pisohamate hiatus, with a portion of this nerve entering the carpal tunnel lateral to the hook of the hamate, solely to rejoin the standard deep ulnar department within the palm. The muscular tissues innervated by the ulnar nerve could also be grouped as follows: forearm group (two muscles), hypothenar group (four muscles), hand intrinsic muscular tissues (three teams of muscles), and the thenar group (two muscles). The flexor carpi ulnaris contracts to stabilize the pisiform in order that the abductor digiti minimi could abduct the fifth digit. The flexor carpi ulnaris contracts to stabilize the pisiform in order that the abductor digiti minimi could perform. The second muscle innervated by the ulnar nerve within the forearm is the flexor digitorum profundus (C8, T1) to the fourth and fifth digits. Branches to this muscle originate when the ulnar nerve is between the flexor digitorum profundus and the flexor carpi ulnaris in the proximal forearm. In 5% of sufferers, branches to the flexor carpi ulnaris originate proximal to the elbow. The superficial sensory division innervates just one, usually forgotten, muscle, the palmaris brevis (C8, T1). To test, immobilize the proximal interphalangeal joint while the patient flexes the distal interphalangeal joint against resistance. The deep motor division offers a small motor branch to the hypothenar eminence simply before diving into the pisohamate hiatus. This department innervates the three muscle tissue of the hypothenar eminence: the abductor digiti minimi, the flexor digiti minimi, and the opponens digiti minimi. One ought to understand that this muscle is delicate, with even regular energy being simply overcome by the examiner. Next, check the opponens digiti minimi (C8, T1) by having the patient maintain the volar pads of the distal thumb and fifth digit collectively. While the patient maintains this place, attempt to force the distal fifth metacarpal away from the thumb. The lumbricals assist flex the metacarpalhalangeal joints and prolong the proximal interphalangeal joints when the metacarpalhalangeal joints are immobilized in a hyperextended position. The palmar interossei adduct or shut the fingers; they also help the lumbricals in flexing the metacarpalhalangeal joints. The deep department of the ulnar nerve innervates the third and fourth lumbricals (to the fourth and fifth digits), in addition to the entire palmar and dorsal interossei muscles. Contraction of the primary dorsal interosseous muscle can be noticed and palpated on the dorsum of the hand. When dorsal interossei muscle losing is current, the extensor tendons on the dorsum of the hand appear more prominent when compared with the conventional hand. Contraction and/or atrophy of the primary dorsal interosseous muscle can be observed and palpated on the dorsum of the hand. Another way to assess the palmar interossei is by having the affected person maintain the prolonged fingers together whenever you try to move a digit between them. The long finger flexors (flexor digitorum superficialis and flexor digitorum profundus) can substitute for digit adduction when the fingers are actively flexed. The finger extensors, in corollary, might help abduct the digits when the fingers are actively prolonged. To eliminate these substitutions and isolate the interossei, the fingers should be in extension on the metacarpalhalangeal joints when assessed. Alternatively, the affected person may be instructed to keep the extended fingers collectively as you try to pass a digit between them (not shown). The second muscle is the deep head of the flexor pollicis brevis (C8, T1), with its superficial head being innervated by the median nerve. Although not a really helpful muscle to test due to its dual innervation, some weak spot compared with the opposite side may be seen with ulnar lesions. Alternatively, you might place your index finger between the thumb and lateral palm, applying resistance as the thumb is adducted (shown).
The lobular cartilage is depressed and the lateral crus is flattened asthma 3 plan advair diskus 100 mcg cheap overnight delivery, much less convex bronchial asthma medical definition advair diskus 100 mcg lowest price, and positioned more caudally asthma and smoking buy advair diskus 250 mcg without a prescription. The later in life surgery is carried out asthma treatment 1920s advair diskus 250 mcg generic on-line, the less negative the consequences will be on further improvement of the nostril and midface. This applies in particular to surgery of the cartilaginous septum and triangular cartilages. The old notion that nasal surgery should be postponed until after puberty is basically nonetheless legitimate. Early repositioning of the septum and cartilaginous pyramid, whereby resections are avoided as a lot as potential, might stop growth of a severely deviated and obstructed nostril during additional growth. It is the task of the nasal surgeon to weigh, in every particular person case, the doubtless advantages of surgery towards the disadvantages. At the chondropremaxillary and perpendicularomeral junction, a pronounced cartilaginous and bony crest and spur are current. A pronounced crest and spur are often present on the chondrovomeral and the perpendicularomeral junction. In such a group, specialists of the following disciplines work together: cosmetic surgery, maxillofacial surgical procedure, otorhinolaryngology, orthodontics, and speech therapy. Here, we focus on only the specific surgery of the septum, pyramid, and lobule in these instances. For surgical procedure of the lip, maxilla, and palate, as properly as the assorted orthodontic options, we refer the reader to other textbooks. Rehabilitation Schedule Most teams deal with a cleft lip patient according to a locally accepted schedule. Such a schedule usually consists of three major phases of rehabilitation: a major section which is carried out within the first yr of life, a secondary section which is performed between four and 10 years of age, and a last phase which is accomplished after puberty (Table 9. Closure of the periosteum of the bony palate and the nasal ground at an early age may inhibit the additional enhance of a number of the anomalies, for example these of the maxillary and premaxillary bones. However, the event of more conservative methods has allowed intervention at an earlier age, if indicated. Repositioning of the septum in childhood could first of all have a helpful effect on nasal respiratory. Whether or not a first section of septal surgical procedure is performed before puberty is dependent upon a quantity of factors, in particular the quality of nasal respiratory. A typical case for early septal correction is the patient with a cleft lip nostril deformity and marked further nasal obstruction because of trauma. Pyramid Surgery Surgery of the bony and cartilaginous pyramid is postponed until after puberty virtually with out exception. Pyramid surgery is often carried out together with secondary septal surgical procedure (and anterior turbinoplasty) as required in the last section of rehabilitation (Table 9. In sufferers with a restricted septal and pyramid deformity, it might be performed in one stage as a part of the correction of the lobule. In different cases, nonetheless, septal and pyramid surgery is carried out first, whereas lobular surgical procedure is completed as one of many ultimate steps some 12 months later. Steps Lobular Surgery Lobular surgery is carried out within the last phase of rehabilitation. This signifies that it might be carried out in the same stage as septal and pyramid correction, or in a separate procedure 1 year after correction of the septum and the bony pyramid. Reconstructing the nasal lobule in cleft lip patients is among the most difficult surgical procedures in nasal surgical procedure, requiring nice skill and expertise. In the past two decades, main closure of the unilateral cleft lip and palate in infancy has not-or solely minimally-involved nasal buildings. Therefore, septorhinoplasty postpuberty in these patients principally means readjustment of the congenitally deformed and distorted nasal buildings, both endonasally or, principally, through an external transcolumellar approach. A transcolumellar inverted-V incision is made together with bilateral infracartilaginous incisions as ordinary within the exterior method. The transcolumellar incision is made as traditional at about one-third of the space from the columellar base. Septoplasty is carried out first and carried out in accordance with the rules and methods described in Chapter 5. A new, straight, septal plate is then extracorporally sculpted and reimplanted, a so-called extracorporal septoplasty (Gubisch 1995). The domes are introduced together by interdomal sutures to achieve a extra slim, projecting and symmetrical tip. Special care is taken to go away a distance of about 1 to 2 mm between the 2 domes. This is completed by suturing its base to the premaxillary fibers by a 4 nonresorbable suture. In case of remaining asymmetry between the 2 domes, a cartilaginous "onlay graft" is fixed on high of the much less outstanding dome. It is characterized by recurrent episodes of upper airway collapse with oxyhemoglobin desaturation and arousals from sleep. This is an important side of the broad area of the brand new specialty, "sleep medicine. A main causative role is irregular dimensions of the higher airway and the oral cavity. Other necessary components are alterations (condition) of the gentle tissues, in particular the mucosa, the nerves and musculature of those areas, and the scale of the adenoids and tonsils. Other causative factors are obesity, alcohol consumption, use of sure medicines, and sleeping position. However, restoration of nasal breathing turned out to have significantly much less impact on loud night time breathing than expected. In some instances, complaints of snoring and apnea have even been discovered to enhance after enhancing nasal respiratory. Nonetheless, there are several indications to deal with nasal obstruction in sufferers suffering from snoring, hypopneas, and apneas. Surgery is carried out primarily as a end result of most patients report a considerable improvement in high quality of life after improvement of nasal respiratory. Hypopneas and apneas are attributable to temporary collapse of a quantity of 334 Special Subjects home equipment (mandibular advancement splints). Nasal surgery is usually adopted by momentary obstruction of the nasal cavities by internal dressings. Even in wholesome folks, inside dressings could trigger hypopneas or apneas and sleep disturbance. Therefore, follow-up of these sufferers by polygraphy or polysomnography is really helpful. However, surgical procedure has a useful effect on snoring and apneas in a restricted number of patients. In basic, snoring is estimated to lower to a socially acceptable level in up to 40% of patients when normal respiration is restored, as proven by research using questionnaires or analog scales. In polysomnographic studies using knowledge from two reviews, it was found to be less than 15% (Table 9. Internal and External Nasal Dilators An inside nasal dilator (Nozovent) that serves to decrease inspiratory breathing resistance and to reduce loud night breathing was launched by Petruson in 1988. At present, no controlled research has demonstrated long-term effectiveness of this system alone in patients Table 9. The same applies to the exterior nasal dilator developed by the three M company beneath the name Breathe Right. Improvements in subjective parameters, similar to subjective sleep high quality, daytime sleepiness, high quality of life, and nonapneic loud night time breathing, have been reported after using nasal dilators. Reviews of subjective and goal data on the effect of nasal dilators have been printed by Rappai et al 2003, Verse and Pirsig 2003, and Rombaux et al 2005. The high air pressure causes an inflammatory response of the nasal mucosa inflicting watery rhinorrhea or a dry nose. In particular instances, maxillomandibular advancement surgical procedure or, very hardly ever, a tracheotomy could be considered.
Advair diskus 100 mcg generic without prescription. HUFF MOVIE TRAILER #2 Windchaser Pictures RealTVfilms.
Actually asthma definition 8k advair diskus 500 mcg purchase otc, it might be more correct to name it a technical failure as a substitute of a complication asthma treatment experiments advair diskus 500 mcg order with visa. The bony and cartilaginous dorsa have been lowered an extreme amount of asthma 7 month old 250 mcg advair diskus, especially within the area of the K area asthma ventilator generic 250 mcg advair diskus with visa. At the same time, some sagging of the cartilaginous dorsum is a typical occurrence as a outcome of insufficient fixation of the cartilaginous septum. A skislope deformity may be prevented by: (1) limiting the amount of reduction of the decrease a half of the bony dorsum; (2) fixating the cartilaginous septum to the premaxilla (or the anterior nasal spine) and the columella to prevent sagging of cartilaginous dorsum; and (3) transplanting some crushed septal cartilage beneath the skin within the K area. If all nasal constructions are involved, we prefer to communicate of a lowwide pyramid syndrome. A bony and cartilaginous saddle nostril is usually corrected by reconstruction of the septum, narrowing and push-up of the bony pyramid following osteotomies, and a dorsal transplant. Low-Wide Pyramid Syndrome Both the bony and the cartilaginous pyramid are severely depressed (see Chapter 2, web page 69). The tip has lost its regular projection, the lobular base is broadened, the alae are more convex or ballooning, and the nostrils are rounded. The septal cartilage is defective or missing as a result of trauma, previous surgical procedure, or infection. As a consequence, the valve area is lowered and widened, and the valve angle is elevated, typically even to 90 In many sufferers, relying on the purpose for the deformity, the mucosa is atrophic, dry, and crusting. The main causes of this syndrome are septal abscess, extreme trauma, congenital anomalies, and particular infections. The surgical method selected for correction will largely depend upon the type and explanation for the saddling or sagging. A "step" may be seen and palpable at the junction of the cartilaginous and bony septum. A bony saddle is relatively rare in contrast with a bony and cartilaginous saddle and cartilaginous saddling. It is normally the outcome of extreme frontal trauma with impression of the bony pyramid. Other attainable causes are illnesses of the nasal bones such as tertiary syphilis and congenital malformations. A bony saddle is corrected by narrowing and push-up of the bony pyramid following osteotomies and insertion of a dorsal transplant. In the heyday of the Killian-Freer submucous septal resection, postoperative sagging of the cartilaginous dorsum was a very common complication. The cartilaginous pyramid could also be reconstructed endonasally in addition to via the external method, relying on the pathology and personal desire. Reconstruction by an onlay of cartilage can very well be carried out endonasally; reworking of the triangular cartilages and narrowing of the cartilaginous vault is best done by the exterior method. The bony pyramid could additionally be mobilized by osteotomies, narrowed and pushed up so far as possible. The lobular cartilages may be dissected and the domes could additionally be sutured collectively to heighten the nasal tip. In abstract, sufferers with major pathology involving all nasal buildings require surgery via an external strategy. Surgery to appropriate restricted pathology, such as cartilaginous sagging or columellar retraction, could additionally be carried out endonasally. We will here discuss the main parts that might be combined in reconstructing a saddle nose. Depending on the pathology, the surgeon has to determine which mixture of the next procedures may be required and efficient in the individual case: 1. Reconstruction of the septum, cartilaginous dorsum, lobular cartilage, and columella using the external method 3. The septum is often faulty, specifically its anterior half, and the cartilaginous pyramid is low and broad, missing normal septal help and projection. The fibrous connections between the cartilaginous and bony pyramid could have been lost, making the decrease margins of the nasal bones seen. The cartilaginous septum has to be reconstructed, positioned in the midline and stuck nicely to its bony base. Many surgeons Endonasal Repositioning and/or Reconstruction of the Septum If the sagging of the cartilaginous dorsum is a complication of previous surgical procedure, we try and appropriate this undesired side impact to begin with by revision septal surgery. We mobilize the septum once more, restore defects (especially these of its cartilaginous part), exorotate the anterior septum, and repair it in its new place. To this end, septopremaxillary sutures, septocolumellar sutures, and splints could also be used (see web page 174 and page 175). Generally, bilateral anterioruperior tunnels and one inferior tunnel are elevated (three-tunnel approach). If desired, the septum can be mounted by including one or two transseptal sutures and/or septal splints. Reconstruction of the Septum, Cartilaginous Dorsum, Lobular Cartilage, and Columella Using the External Approach this is the preferred procedure in instances with severe pathology, as it allows correction of all anatomical buildings. The anterior a half of the cartilaginous septum is dissected each from under (dissection starting at the caudal end) and from above. The triangular cartilages are uncovered (extraperichondrially) and the valve angle is freed. The domes and the lateral crura of the lobular cartilages are dissected out extraperichondrially as a lot as required for redraping. Stabilization of the septum on the nasal backbone and/or the premaxilla is of utmost significance, as the standard of the septal reconstruction tremendously determines the practical and aesthetic end result. The triangular cartilages are sutured to the ventral margin of the septum to get hold of stability. The medial crura may be mounted to the caudal end of the septum by two or three 5 sutures. This significantly adds to the stability and prominence, but might trigger a sure stiffness of the lower third of the nasal pyramid. Depending on the result obtained by the earlier procedures, a cartilaginous transplant could also be required to get hold of a straight dorsum (see below). If a more voluminous transplant is required, a sculpted transplant from septal, auricular, or rib cartilage is used. Care is taken that no perichondrium is left hooked up to keep away from progress of the transplant. After insertion, the transplant is molded into place with the fingers and glued by external taping. Noncrushed Septal Cartilage or Auricular Cartilage In patients with a moderate melancholy of the cartilaginous pyramid, a single or double transplant of noncrushed septal cartilage, or of auricular cartilage with perichondrium hooked up on one side, is a typically accepted method of augmentation. Augmentation of the dorsum by a transplant is carried out as a further process. The short-term outcomes of auricular grafts in circumstances with moderate sagging are satisfactory. In the lengthy run, nevertheless, a certain quantity of resorption (rather variable in our experience) will take place. Instead of auricular cartilage, one could use a graft sculpted from septal cartilage. Narrowing and Push-Up of the Bony Pyramid A bony saddle could also be decreased by narrowing and pushup of the bony pyramid following mobilization of the pyramid by osteotomies. Because crushed septal cartilage is simple to mould, it makes an nearly ideal transplant material. The amount of resorption is estimated at 30 to 60%, depending on the diploma of crushing. Crushed septal cartilage is due to this fact only used to appropriate a limited the transplant is taken from the auricle reverse the side on which the affected person prefers to sleep. We like to resect the transplant by the anterior approach; others use the posterior one.
Involvement of very proximal branches of the brachial plexus asthma trailer order advair diskus 500 mcg without a prescription, together with the phrenic nerve (paralyzed hemidiaphragm) nocturnal asthma definition generic advair diskus 250 mcg visa, dorsal scapular nerve (rhomboid weakness) asthma 50 lung capacity buy generic advair diskus 100 mcg online, and long thoracic nerve (scapular winging) additionally suggests preganglionic harm asthma bronchitis natural cures advair diskus 100 mcg, or at least intraforaminal injury. Avulsion of the T1 spinal nerve can cause Horner syndrome, the presence of which must be readily apparent on examination. With this type of injury, the peripheral nerve sensory axons stay linked to their cell our bodies in the spinal ganglia. Therefore, the amplitudes of distal extremity sensory nerve motion potentials remain regular (or increased), regardless of no sensation being present on examination. The presence of compound motor action potentials argues in opposition to spinal wire avulsion. Paraspinal denervation can be indicative of preganglionic or intraforaminal nerve damage. My examination routine is divided into six distinct steps (See Box: Six steps of a complete brachial plexus examination (p. Six steps of a comprehensive brachial plexus examination Back Observation Rhomboids Latissimus dorsi Trapezius Scapular winging Shoulder Supraspinatus Deltoid Posterior deltoid Teres major Pectoralis main Infraspinatus Arm Triceps Biceps Brachioradialis Forearm Supinator Pronator Wrist flexion Wrist extension Finger extension Hand Observation Finger flexion 132 Clinical Evaluation of the Brachial Plexus Thenar intrinsics Hypothenar intrinsics Interossei Lumbricals Skin Sensation Perspiration/Horner syndrome Pulses/masses Reflexes/Tinel sign Step 1: Back. The presence at remainder of scapular winging, muscle atrophy, and asymmetry of the shoulders and scapulae are famous. Next, the patient shrugs the shoulders upward to allow assessment of trapezial and levator scapulae operate. Having the affected person convey the scapulae together permits evaluation of the rhomboids. The latissimus dorsi are palpated bilaterally, and the affected person is requested to cough, which causes their contraction. The patient is instructed to raise the arms to the aspect and straight above the head to check trapezial perform. Next, the affected person is informed to attain toward the wall with the affected arm, and scapular winging is evaluated. Starting with the arm straight and to the side, the patient is instructed to abduct the arm. With the arm horizontal to the floor, the posterior head of the deltoid (posterior movement) and teres major (downward movement) are examined. The affected person then flexes the forearm ninety degrees ("hold-up" position), and both the clavicular (lateral pectoral nerve) and sternal (medial pectoral nerve) heads of the pectoralis major are assessed, each visually and by palpation. The triceps are examined with the upper arm parallel to the floor, so the impact of gravity is eliminated. Elbow flexion is tested with the forearm both fully supinated (biceps brachii) and half supinated (brachioradialis). The patient flexes the wrist (flexor carpi radialis and ulnaris), after which the arm is pronated and the wrist extensors are tested (extensor carpi radialis longus and brevis and extensor carpi ulnaris). With the forearm positioned on a flat floor, the long forearm finger extensors (extensor digitorum communis, extensor indicis, extensor digiti minimi, and extensor pollicis longus and brevis) are evaluated. The affected person is then instructed to open and close the hand so that any evidence of contracture can be observed, if present. Next, the thumb is evaluated additional, together with abduction, adduction, opposition, and flexion. Flexion on the proximal (flexor digitorum superficialis) and distal (flexor digitorum profundus) interphalangeal joints is assessed. Abduction and opposition of the fifth digit are evaluated, in addition to any Wartenberg or palmaris brevis signs. Finger abduction (dorsal interossei), adduction (palmar interossei), and extension on the interphalangeal joints are tested (lumbricals). Fingertip testing is very essential, considering that the thumb, long finger, and fifth digit symbolize totally different dermatomes. Any abnormality or asymmetry between the upper extremities is evaluated further, together with evaluation of two-point discrimination and localization. This emergent analysis, nonetheless, is often limited by other injuries, including long-bone fractures, spine trauma, and affected person confusion or stupor. This screening examination, or main survey, evaluates 9 muscular tissues that have been selected as a outcome of they every comply with a separate path via the brachial plexus (Table 5. Finally, hand movements are examined, including the flexor carpi radialis, extensor indicis, abductor pollicis brevis, and dorsal interossei. If the first survey reveals a deficit, a secondary survey in the emergency department includes sensory and additional motor testing. Proximal lesions are then tested using a spinal nerve template (which spinal nerves are affected To perform the secondary survey, consider all the muscle tissue innervated by the injured factor (as determined by the first survey. A complete examination (described previously) ought to all the time be performed; nevertheless, in many trauma sufferers, that is completed later when the patient is fully cooperative and more time is on the market. Other, much less frequent etiologies include compression by anomalous fibrous ridges on the scalene musculature (neurogenic thoracic outlet syndrome), a hundred thirty five Clinical Evaluation of the Brachial Plexus delayed radiation injury, and acute brachial plexitis (Parsonage-Turner syndrome). The supply of irritation for neurogenic thoracic outlet syndrome is localized to the scalene triangle. The scalene triangle is made up of the anterior scalene anteriorly, the middle scalene posteriorly, and the sting of the primary rib inferiorly. Irritation of the brachial plexus is usually from an irregular fibrous band, on or near these two scalene muscle tissue. An elongated C7 transverse course of or cervical rib may be present, both of which unfavorably reorient the scalene muscles, probably resulting in neural compression or irritation. The patient with classic neurogenic thoracic outlet syndrome has forward-drooping shoulders. Manifestations of neurogenic thoracic outlet syndrome are normally localized to the C8 and T1 spinal nerves. Sensory loss, when present, occurs on the medial side of the forearm, as properly as on the medial third of the hand. Hand intrinsic weak spot and atrophy are often more median than ulnar, whereas sensory loss is all ulnar (ulnar and medial antebrachial cutaneous nerves, both from the medial cord). Externally rotating the arm while abducting it above the pinnacle typically precipitates or worsens symptoms after a minute or two in this place (Roos maneuver or elevated arm stress test). An apical lordotic cervical radiograph paperwork a cervical rib or elongated C7 transverse process, when present. Care must be taken to differentiate thoracic outlet syndrome from C8 radiculopathy or ulnar compression on the elbow. Concurrent weak point in median (abductor pollicis brevis) in addition to ulnar (abductor digiti minimi or the first dorsal interosseous) innervated muscular tissues helps confirm a extra proximal damage to the brachial plexus. No history of neck or radicular ache, together with the presence of both C8 and T1 sensory and motor changes, helps exclude a single-level radiculopathy. The most typical harm is an Erb palsy, the place C5 and C6 (or the upper trunk) are damaged. Another type of delivery injury is Klumpke palsy, with harm to the C8 and T1 nerve roots. Although this palsy can occur throughout a breech delivery, with the arm hyperabducted above the head, it mostly happens after a face-first supply where the top is hyperextended. Other kinds of birth brachial plexus harm embrace complete plexal harm and an Erb plus palsy. The prognosis of both Klumpke palsy and full brachial plexus palsy are considerably worse than that for Erb palsy. Neurological diagnosis of an obstetrical palsy depends significantly on observing the arm and hand position at relaxation, a scarcity of motion, and higher extremity asymmetry throughout play and crawling. Electrodiagnosis should be first carried out four to 6 weeks after damage, and then on a serial basis (approximately every 3 months) to assess restoration. As the child grows, the neurological examination turns into more structured, including various arm actions of functional significance. A frequent position of comfort is the arm adducted and elbow flexed, the so-called adduction-flexion sign of acute brachial plexitis. Weakness is normally not present through the acute, painful section of this syndrome; nonetheless, because the pain resolves, paralysis of sure brachial plexusinnervated musculature happens.