
Geodon
| Contato
Página Inicial

"Order geodon 80mg free shipping, anxiety zone thyroid".
E. Arokkh, MD
Assistant Professor, Hackensack Meridian School of Medicine at Seton Hall University
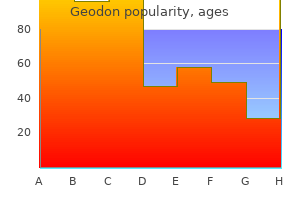
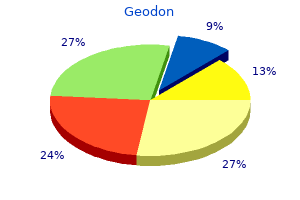
Robotic and laparoscopic repairs utilizing the same rules as open restore have been reported (Miklos et al mood disorder nos dsm iv purchase 80mg geodon amex. Antegrade nephrostogram demonstrates gentle ureterectasis with opacification of the vagina (arrow) depression hormone test 80mg geodon generic with visa. In this clinical setting mood disorder group activities geodon 80mg discount amex, which generally happens after vaginal supply depression just want to sleep 20 mg geodon discount otc, urine flows from the bladder via the fistula into the uterine cavity after which into the vagina through an incompetent cervical os. However, in the setting of a related medical history, vesicouterine fistulae additionally manifest with menouria and cyclic hematuria within the setting of urinary continence. Youssef syndrome describes the presenting symptom advanced of vesicouterine fistula: menouria, cyclic hematuria with associated apparent amenorrhea, infertility, and urinary continence (Youssef, 1957) in a patient who has undergone prior low-segment cesarean section. Endometriosis of the bladder by which cyclic hematuria may be present must be differentiated from this situation. Successful restore of ureterovaginal fistulae is anticipated in additional than 90% of instances. All patients were cured utilizing a mix of techniques together with the Boari flap. Ureterouterine fistulae might happen because of cesarean section, uterine malignancy, and elective abortion (Billmeyer et al. Uretero�fallopian tube fistulae have additionally been reported as a consequence of laparoscopic fulguration of endometriosis (Chene et al. Diagnosis and Management Diagnosis of vesicouterine fistula may be made by a mixture of cystoscopy and radiographic research, though a excessive diploma of suspicion is important to pursue the diagnosis if initial radiographic studies show adverse (Smayra et al. Several different approaches have been advocated for the remedy of vesicouterine fistulae. Prolonged indwelling bladder catheterization or fulguration of the fistula tract adopted by bladder drainage may be successful in select instances, particularly in sufferers with small, immature fistulae (Graziotti et al. Hormonal induction of menopause will induce involution of the puerperal uterus, and this principle has been used with some success in treating this situation as nicely (Ravi et al. Jozwik and Jozwik (1999) reported profitable treatment in eight of 9 patients with use of hormonal manipulation. Surgical therapy for vesicouterine fistulae is usually contingent on the precise reproductive wishes of the affected person, as properly as other surgical factors, however is considered definitive remedy. Vaginal repair is feasible in chosen sufferers, however many would require an abdominal strategy (Milani et al. For the affected person who needs preservation of fertility, uterine-sparing surgery may be thought-about. However, the incidence of this situation is growing in parallel with the rising numbers of low-segment cesarean sections being accomplished worldwide (Kumar et al. Cesarean part is by far the most typical cause of this unusual fistula (Tancer, 1986). Tancer associated that of the 74 cases of vesicouterine fistulae reported from 1947 to 1986, fifty seven adopted low-segment cesarean section, 7 adopted vaginal operative delivery, and the remaining instances were related to quite a lot of disparate scenarios, together with induced abortion, hysterectomy, and dilation and curettage (D&C). Vesicouterine fistulae might happen spontaneously because of a ruptured uterus throughout obstructed labor. In these cases, the posterior bladder wall could tear along the uterine rupture line creating the potential for a fistula. Bladder wall invasion by chorionic villi penetrating past the uterine serosa, placenta percreta, may also create a vesicouterine fistula (Krysiewicz et al. In most circumstances, simultaneous damage to the bladder and uterus is the inciting event. An unrecognized and unrepaired (occult) bladder damage, or incorporation of a portion of the bladder during closure of the uterus throughout any number of operations, might lead to a vesicouterine fistula. Anatomically, the most typical location of the fistula is alongside the posterior bladder wall in the midline, or from the genital side, just cephalad to the internal cervical os. Ureteral stents can be positioned to facilitate identification of the ureters intraoperatively. After efficiency of the hysterectomy, the fistula tract on the posterior bladder wall is excised and the bladder is closed primarily. Hysterectomy adopted by repair of the bladder is indicated for the individual who now not needs fertility. Uterine-sparing procedures can be used, and successful pregnancy is feasible after vesicouterine fistula restore. Computed tomography scan with distinction enhancement demonstrating a vesicouterine fistula. Contrast materials is layering within the partially crammed urinary bladder; contrast opacification of the uterine canal suggests a vesicouterine fistula. In industrialized nations urethrovaginal fistulae in adults mostly have an iatrogenic cause. In feminizing genital reconstructions in youngsters with ambiguous genitalia and surgical repairs of cloacal malformations, urethrovaginal fistulae can occur as early or late complications (Dhabalia et al. Also in transsexual adults undergoing feminine to male reconstruction, urethrovaginal fistulae have been reported (Hage et al. Careful dissection permits separation of the bladder from the uterus beyond the fistula tract. The fistula tract is excised from each buildings, the uterus and bladder are closed individually, and an interpositional flap, often omentum, is secured between the two organs (Sapmaz et al. Minimally invasive laparoscopic and robotic surgical approaches to the restore of vesicouterine fistulae have been reported (Alamoudi et al. In the surgical therapy of stress incontinence in girls with bulking brokers (Carlin and Klutke, 2000; Hilton, 2009) or synthetic slings a number of instances of urethrovaginal fistulae have been reported (Blaivas and Mekel, 2014; Estevez et al. Even conservative remedy of prolapse with pessaries can result in the formation of fistula, if these pessaries are neglected for an extended time frame, although fistula formation after solely 2 weeks of pessary use has been described (Hilton and Cromwell, 2012; Walker et al. Trauma, including inappropriate catheterization, and foreign our bodies are apparent causes of fistulae (Blaivas and Purohit, 2008; Cameron and Atiemo, 2009; Holland et al. Urethral diverticulae and their surgical repair can also result in urethrovaginal fistulae (Ben Amna et al. Urethrovaginal fistulae have additionally been described in some Beh�et sufferers with vasculitis and local necrosis of the urethrovaginal septum (Chung et al. Other causes of urethrovaginal fistulae include trauma (including pelvic fracture) and vaginal neoplasms. A final necessary trigger in the long-term�care setting is urethral catheter erosion (Andrews and Shah, 1998; Trop and Bennett, 1992). In patients with poor sensation, particularly the cognitively or otherwise neurologically impaired affected person, pressure necrosis from a chronically indwelling catheter may result in traumatic hypospadias and urethrovaginal fistula. For that purpose suprapubic catheters are to be most popular in sufferers with cognitive and/or neurologic impairment. Symptoms of urethrovaginal fistulae are largely depending on the size and site of the fistula alongside the urethral lumen. A small fistula might produce solely minimal leakage, whereas a big urethrovaginal fistula could cause steady urine drainage. Distal fistulae past the sphincteric mechanism could also be fully asymptomatic or may be related to a splayed urinary stream. Severe complete erosion of the urethra secondary to persistent indwelling urinary catheter. This affected person with advanced a quantity of sclerosis underwent surgical bladder neck closure and ileovesicostomy (ileal chimney). This affected person was referred for the analysis of persistent incontinence after urethral diverticulectomy. A voiding cystourethrogram demonstrates incomplete resection of the urethral diverticulum (white arrow) with a pinpoint postoperative urethrovaginal fistula (black arrow shows a small quantity of contrast material faintly outlining the anterior vaginal wall). Resection of the residual diverticulum with restore of the fistula by a Martius flap was healing. Urethrovaginal fistula on lateral voiding picture from voiding cystourethrography demonstrates fistula (black arrow) on this affected person with a major symptom of vaginal voiding. However, due to its brief length, the female urethra could additionally be tough to absolutely look at with a regular rigid cystoscope, because the irrigation fluid is discharged 1 to 2 cm proximal to the lens. Passage of a flexible wire endoscopically from the urethral lumen into the vagina can assist in finding the fistula tract. In some instances more superior methods are used to shut or to shield the urethral closure. In circumstances of adverse dissection and visualization, urethral sectioning has been advocated (Parks, 1965).
One try of blind catheterization with a Tiemann tip catheter may be performed depression era glass buy geodon 80mg lowest price, but this try should be aborted in case of any problems depression worse at night order 80mg geodon amex. A second attempt could be performed with the use of a Freudenberg mandarin by which the sharp curve at the native feminine urethral meatus may be handed easily depression symptoms worksheet geodon 20mg purchase. In the early postoperative period anxiety at night 40 mg geodon buy fast delivery, the fistula is clear if the urethral catheter is visible by way of the wound dehiscence. For this function, the urinary diversion (transurethral or suprapubic catheter) is maintained till this problem is resolved. After this era, the urinary diversion can be eliminated, and the affected person can begin to void via the fistula. Smaller fistulas have a high probability (up to 70%) of spontaneous closure (Monstrey et al. The fistulous tract is excised with closure of the urethra and pores and skin and with interpositioning of a healthy layer between both. As no dartos layer is available in these sufferers, only native fatty tissue can be utilized for coverage. Compared with the male urethra, which consists of mucosa in spongiosal tissue, the phallic urethra relies on pores and skin from the flap in which therapeutic is delayed. Again, stricture formation is normally associated to therapeutic problems of the phallus and mostly occurs at areas with a poorer blood supply. This is the rationale why the vast majority of strictures are situated on the phallic part of the urethra, the anastomosis, or the exterior meatus (Lumen et al. Most of the strictures at the anastomotic website are quick and will normally appear brief after phallic reconstruction. As in males, transmen with urethral stricture will present with a typical plateau curve on uroflowmetry. Urethral Complications in Transmen Up to 40% of sufferers will suffer urethral complications after phalloplasty. Urethral Fistula A urethral fistula is a very common early postoperative complication (35%) (Monstrey et al. The commonest location is on the base of the phallus adopted by fistulae on the shaft of the phallus. Perineal fistulae are uncommon due to the higher coverage of the urethra with Chapter 134 Special Urologic Considerations in Transgender Individuals 3071 Endoscopic incision has a success price of 44%. The sooner after phallic reconstruction, the decrease the prospect of success (Lumen et al. Urethral Reconstruction Native urethra Urethral reconstruction is carried out for short (<3 cm) strictures refractory to dilation or endoscopic incision and for longer strictures at any phase of the urethra in transmen. Compared with urethral reconstruction in native males, the next recurrence fee is observed (25% to 61. The ventral aspect of the stenotic meatus in incised till wholesome urethra is reached. Meatus Heineke-Mikulicz Urethroplasty this is an option for short, nonobliterative strictures at any phase of the urethra. The three components of the urethra (native feminine urethra, perineal urethra or mounted half, and phallic urethra) in transmen after phalloplasty as seen on retrograde urethrography. Excision and Primary Anastomosis this is reserved for short strictures on the anastomotic web site between the fixed and the phallic part of the urethra. A steel sound is introduced via the meatus and marks the distal finish of the stricture. The urethra is incised ventrally and further opened until wholesome proximal urethra on the mounted part is encountered. In case of full obstruction, the proximal finish of the stricture may be marked by passing a metal sound by way of the perineostomy or the suprapubic tract. The stenotic phase is totally resected, and each urethral ends are spatulated. Any form of remedy of urethral stricture illness should be postponed for at least 3 months and preferably 6 months after phallic reconstruction, at the time wound therapeutic of the phallus has stabilized. It is useless to carry out reconstruction during the acute phase of irritation and wound therapeutic. In case of invalidating obstructive symptoms or retention, a suprapubic catheter is inserted as first-line remedy. A perineostomy is an option if a long interval for definitive urethral reconstruction is expected, in case of severe complaints associated to the suprapubic catheter. This perineostomy could be closed at the time of urethral reconstruction or in a later phase if the urethral reconstruction appears to achieve success. The type of remedy is determined by earlier interventions, stricture location, stricture size, and concomitant problems associated to the phallus. At the fastened part, a graft could be positioned after incision of the urethral plate as a dorsal inlay procedure. The need for this method is, nevertheless, exceptional seen the low incidence of stricture at this website. Urethral Dilation Intermittent urethral dilation is an possibility for low-grade meatal stenosis. A single dilation is feasible for a short flimsy stricture at the anastomosis between the phallic and fixed part. This dilation is preferably accomplished with fluoroscopic steering to keep away from creating a false passage at the urethra. Two-Stage Urethroplasty it is a standard method to deal with longer strictures at the phallic urethra. The urethra is opened, and marsupialization is obtained by suturing the borders of the urethra to the borders of the skin incision. In case of a narrow and/or severely scarred urethral plate, the plate may be resected and replaced or augmented by a full-thickness skin graft or by oral mucosa. At least 3 months later, if the urethral plate has healed nicely, the borders of the marsupialized urethra are incised and retubularized round a urethral catheter. Flap Urethroplasty Substitution urethroplasty with native phallic or scrotal skin flaps is of limited use seen the paucity of mobile native tissues and the chance for penile/scrotal deformities after native flap harvest. For complicated or recurrent stricture at the phallic urethra, a complete urethral substitution at this part needs to be performed. Options are a radial forearm free flap or a superficial circumflex iliac artery free or pedicled groin flap. They can current themselves to each urologist with urologic problems, which is why perception into the reconstructive strategies and potential problems is helpful for every urologist. The goal of this chapter was to present any urologist with important knowledge to have the flexibility to take care of acute urologic problems. Thereafter, referral to experienced centers for therapy of the issues is advisable. Definitive Perineostomy the approach is similar as for contemporary perineostomy within the early postoperative phase. The perineum is incised on the midline until the mounted a half of the urethra is reached. Urethral Hair Growth In case the urethra is made from pores and skin flaps (which is normally the case), hair development can occur in the urethra. If a pores and skin flap might be used for the phallic urethra, a flap from a area with no or minimal hair development is harvested. Related signs are difficulty voiding, local irritation, and urethral discharge. Once it has formed, the phallic urethra is opened on the ventral side with removal of the stone (if present). The borders of the urethra are sutured to the borders of opened pores and skin of the phallus. In the next stage, the urethral plate is tubularized as through the second stage of a two-stage urethroplasty. De Cuypere G, Knudson G, Bockting W: World Professional Association for Transgender Health: mission and Vision. Weyers S, De Sutter P, Hoebeke S, et al: Gynaecological elements of the therapy and follow-up of transsexual men and women, Facts Views Vis Obgyn 2(1):35�54, 2010. Postvoid Dribbling Nearly all transmen will expertise some form of postvoid dribbling (Hoebeke et al.
China-Wood Oil (Tung Seed). Geodon.
- How does Tung Seed work?
- Dosing considerations for Tung Seed.
- What is Tung Seed?
- Asthma, bowel problems such as diarrhea and constipation, and other conditions.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96371
Indeed depression symptoms journal articles discount geodon 80mg line, elimination of main segments from the alimentary tract may cause nocturnal bowel actions mood disorder program purchase 40 mg geodon visa, fecal urgency depression self help geodon 40mg safe, fecal incontinence river depression definition geodon 40 mg online buy cheap, diarrhea, and dietary deficiencies (Riddick et al. A examine compared sufferers with ileal conduits with those who had segments used for clam cystoplasty and, not shocking, found that those with clam cystoplasty had a 40% incidence of serious bowel issues. Thus,there isa want for heightened consciousness of bowel dysfunction in sufferers with detrusor instability in whom bowel segments are to be used. A examine of sufferers who had an ileocystoplasty famous that 7% had significant diarrhea (Blaivas et al. One should warn patients who will have major parts of the intestinal tract used in the reconstruction that bowel issues could ensue. Cancer the incidence of cancer improvement in patients with ureterosigmoidostomy varies between 6% and 29%, with a mean of 11% (Schipper and Decter, 1981; Stewart etal. On histologic examination, the tumors embrace adenocarcinoma, adenomatous polyps, sarcoma, and transitional cell carcinoma. Case reports of tumors developing in sufferers with ileal conduits, colon conduits, bladder augmentations, rectal bladder, neobladders, and ileal ureters have been described (Austen and K�lble, 2004). Anaplastic carcinomas and adenomatous polyps have been reported in patients with ileal conduits. Adenocarcinoma has developed in patients with colon conduits; adenocarcinoma, undifferentiated carcinoma, sarcomas, and transitional cell carcinomas have developed in patients with bladder augmentations with both ileumandcolon(Filmer,1986). Whether the tumor arises from transitional epithelium or colonic epithelium is unclear. Because a lot of the tumors are adenocarcinomas, it has been assumed that the tumor arises from the intestinal epithelium. Adenocarcinomas have been proven to arise from transitional cell epithelium exposed to the fecal stream in experimentalanimals(Aaronsonetal. Furthermore,studies show that the ureters in ureterosigmoidostomy patients have an exceedingly excessive incidence of dysplasia (Aaronson and Sinclair-Smith, 1984). This is illustrated by a case report during which a patient who had a ureterosigmoidostomy that was defunctionalized with a conduit subsequently developed most cancers 9 months later. This suggests that when ureterointestinal anastomoses are defunctionalized, they want to be excised quite than merely ligated and left in situ. Other proof including cell staining strategies suggests that the colon is the first organ of origin (Mundy, personal communication, 1991). Whether the urothelium or intestine is the first web site of origin, it seems probably that tumors can come up from each tissues. The highest incidence of cancer happens when the transitional epithelium is juxtaposed to the colonic epithelium and each are bathed by feces(Shandsetal. An irregular pattern of colonic mucin secretion has been demonstrated in sufferers with ureterosigmoidostomy, but its significance is unclear (Iannonietal. Ornithine decarboxylase, an enzyme that has been found to be elevated in malignant colonic mucosa, can be elevated in experimental animals with vesicosigmoidostomy (Weber etal. The position of epidermal progress factor and different development elements is currently being investigated. Evidence means that these might a minimum of play a role in growth, if not in induction. Thus theoretically, for a given wall pressure, the greater the radius, the smaller the generated strain. This is desirable in an try and forestall deterioration of the upper tracts or incontinence. Rather, the bowel demonstrates viscoelastic properties, which are likely to distort the connection between pressure utilized on the wall and pressure generated in it. However, even though the mathematical modeling is complex, it seems desirable to try and construct as spheric a container as attainable if one is trying to make a reservoir. For ileal pouches, it has been proven that the capability increases sevenfold after 1 12 months (Berglund etal. As a end result, the authors recommended common endoscopic analysis starting 5 years postoperatively for these patients, but not for patients with ileal neobladders (0. The authors additionally beneficial that sufferers with catheterizable ileocecal pouches (0. Neuromechanical Aspects of Intestinal Segments Both small bowel and colon contract to propel luminal contents in an aboral path. The ability to propel luminal contents is a consequence of muscle activity and coordinated nerve activity. Both the small bowel and the colon have an outer longitudinal layer of muscle and an inside circular layer. There can be a muscularis mucosa, which is immediately beneath the mucosa and should prolong into the villi. The outer and internal layers of muscle, nonetheless, play the main role in peristalsis. In the colon, the outer longitudinal layer of muscle condenses to type three taeniae coli. The enteral nervous system operates autonomously, and subsequently one can denervate the gut and never have an effect on the coordinated contractions. These contractions are termed activity fronts and could also be stimulated by feeding, or they might be inhibited by publicity of the lumen to varied substances. Two elements of neuromechanical properties are notably germane to urinary intestinal diversion: volume-pressure relationships and motor activity. Volume-Pressure Considerations the volume-pressure relationships depend on the configuration of the bowel. In reconstruction of intestinal segments for the urinary tract, nonetheless, one must close the ends. Indeed, the larger the ratio Motor Activity It has been advised that splitting the bowel on its antimesenteric border discoordinates motor exercise and thereby causes a lesser intraluminal strain. Clearly, the perfect situation is to present the patient with a spheric vessel that has few or ineffective contractions of its walls. Thishasalso been demonstrated clinically; initially after reconfiguration of the bowel (detubularization), coordinated activity fronts have been proven to lower. The literature is contradictory with respect to the impact of detubularization on segments of ileum and colon used to construct storage vessels for continent diversions. When the 2 segments are positioned collectively, the circumference is doubled, thus doubling the volume. Closing the ends of the cylinder requires a reduction in its size equal to the radius of the tip. Pressure waves recorded 1 year postoperatively in a patient with a continent diversion constructed from detubularized ileum and right colon. Note that the coordinated stress waves are of magnitude and frequency similar to these present in a traditional colonic or ileal phase. Because the bowel wall is freely permeable to water, the upper osmotic content of urine obligates movement of water into the bowel lumen. Also, as indicated earlier, early reports of detubularized segments could be anticipated to differ from later stories when coordinated exercise fronts in these segments return. Detubularization of ileal segments has been reported by some to lower motor exercise at 1 12 months in contrast with immediately postoperatively(Berglundetal. Ileumhas additionally been proven to have fewer activity fronts per unit of time than cecum (Berglund etal. Cecum has been noticed to have the identical number of exercise fronts 1 year postoperatively, but the amplitude of the pressure waves has been observed to decrease over time(Hedlundetal. TheMainz pouch, which uses both ileum and cecum, has an average strain at capability of 39 cm H2O with a most pressure of 63 cm H2O (Th�roffetal. Thus, reconfiguring bowel normally increases the amount, but its long-term effect on motor activity and wall rigidity is unclear right now. It has been our observation that some sufferers with orthotopic bladders, after a variety of years of spontaneous voiding, require intermittent catheterization. In these patients, the bowel section has turn into flaccid, and the ability of the patient to generate intraluminal strain by the Valsalva maneuver is proscribed. Moreover, the procedure preceding the urinary intestinal diversion additionally has a set of complications that must be added to those described earlier.