
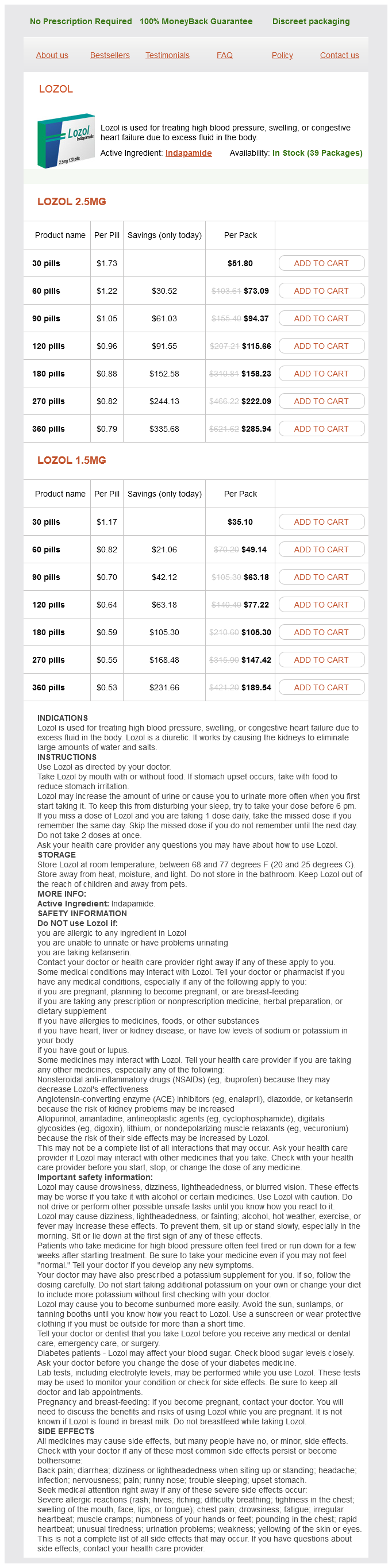
Indapamide
| Contato
Página Inicial
"Safe 1.5 mg indapamide, blood pressure device".
E. Uruk, M.B. B.CH., M.B.B.Ch., Ph.D.
Clinical Director, Texas Tech University Health Sciences Center Paul L. Foster School of Medicine
Regimens are likely to heart attack at 25 2.5 mg indapamide generic with amex be center-specific dependent on local antibiotic sensitivities prehypertension 126 1.5 mg indapamide with amex, however should include gram-negative cowl by a third era cephalosporin or aminoglycoside and gram-positive cover by vancomycin or a cephalosporin arteria pharyngea ascendens buy indapamide 1.5 mg amex. In polymicrobial peritonitis heart attack 02 50 heart attack enrique iglesias s and love generic indapamide 1.5 mg without a prescription, notably in association with anaerobic micro organism, the danger of death is elevated, and an pressing surgical evaluation ought to be sought as a outcome of early laparotomy might cut back mortality. However, there are circumstances where catheter removal is required, as outlined in Table 5. The majority of patients undergo laparotomy and catheter elimination, with concomitant peritoneal washout. However, laparoscopic elimination and washout has been shown to be as effective as the open method, but associated with less postoperative pain and bowel dysfunction. Prolonged makes an attempt to medically treat refractory peritonitis are related to extended hospital stay, peritoneal membrane damage, increased danger of fungal peritonitis, and demise. Diagnosis can be troublesome, however must be suspected in the presence of persistently elevated mononuclear cell counts with unfavorable cultures. Acid-fast bacilli smears of dialysate fluid may be negative in 90% of circumstances, but formal cultures are usually constructive. Mortality attributed to tuberculous peritonitis is around 15%, and much of this may relate to treatment delay. Patients may current with abdominal ache, a decline in internet ultrafiltration, ascites, bloody effluent (7%�50%), bowel obstruction, vomiting, malnutrition, or an stomach mass. Ultrasonography could reveal bowel wall thickening, a thick-walled mass containing bowel loops, loculated ascites, and fibrous adhesions. Surgery to remove all fibrotic tissue and free the bowel is a major undertaking, with a imply operative time of 7 hours and a mortality of round 7%. However, bowel operate is restored in 96% of patients, though 25% of sufferers would require repeat surgical procedure. To attempt to stop recurrence sufferers could also be treated with immunosuppressive agent postoperatively, mostly corticosteroids. Restoration of patency in failing tunneled hemodialysis catheters: a comparability of catheter exchange, change and balloon disruption of the fibrin sheath, and femoral stripping. Subclavian vascular entry stenosis in dialysis patients: pure history and danger components. Post-catheterization venous stenosis in hemodialysis: comparative angiographic research of fifty subclavian and 50 internal jugular accesses. An outcomes comparison of native arteriovenous fistulae, polytetrafluorethylene grafts, and cryopreserved vein allografts. Autogenous versus prosthetic vascular access for hemodialysis: a systematic evaluation and meta-analysis. Outcomes of brachiocephalic fistulas, transposed brachiobasilic fistulas, and upper arm grafts. Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: a randomized managed trial. Hemodialysis arteriovenous fistula patency revisited: outcomes of a potential, multicenter initiative. Outcomes of vascular entry for hemodialysis: a systematic review and meta-analysis. The organisation and supply of the vascular entry service for upkeep haemodialysis patients. A randomized managed trial and cost-effectiveness evaluation of early cannulation arteriovenous grafts versus tunneled central venous catheters in patients requiring pressing vascular access for hemodialysis. A strategy for rising use of autogenous hemodialysis entry procedures: impact of preoperative noninvasive evaluation. Effect of preoperative sonographic mapping on vascular access outcomes in hemodialysis sufferers. In deceased donor transplant recipients catheter removal should be as early as is feasible. Routine removing at four weeks in sufferers with a functioning transplant minimizes potential infections. Conclusion Optimal bodily and psychological well being for the dialysis patient could be achieved by multidisciplinary care, and central to this is effective dialysis entry. Early planning of entry procedures permits a easy transition from predialysis to dialysis and minimizes the utilization of momentary venous catheters. Furthermore, efficient dialysis access provides a lifeline for an ever-increasing group of sufferers in whom transplantation is deemed unsuitable. Relationship between blood flow in central venous catheters and hemodialysis adequacy. Mediastinal strategy to the position of tunneled hemodialysis catheters in sufferers with central vein occlusion in an outpatient access heart. Outcomes of arteriovenous fistula creation, impact of preoperative vein mapping and predictors of fistula success in incident haemodialysis sufferers: a single-centre expertise. Effect of regional versus native anaesthesia on consequence after arteriovenous fistula creation: a randomised controlled trial. Regional versus local anaesthesia for haemodialysis arteriovenous fistula formation: a systematic evaluation and meta-analysis. Arteriovenous fistulae for haemodialysis: a systematic review and metaanalysis of efficacy and safety outcomes. Brachiobasilic versus brachiocephalic arteriovenous fistula: a prospective randomized examine. Videoscopic basilic vein harvest for creation of transposed brachiobasilic arteriovenous fistulae. Patency of autogenous and polytetrafluoroethylene upper extremity arteriovenous hemodialysis accesses: a scientific evaluate. Associations between hemodialysis entry sort and clinical outcomes: a systematic review. Long-term outcomes of fistula first initiative in an city college hospital-is it still relevant The effect of location and configuration on forearm and higher arm hemodialysis arteriovenous grafts. Subclavian vein to proper atrial appendage bypass without sternotomy to preserve arteriovenous access in patients with full central vein occlusion, a new approach. An arterioarterial prosthetic graft instead option for haemodialysis entry: a scientific evaluation. Medial fibrosis, vascular calcification, intimal hyperplasia, and arteriovenous fistula maturation. Pre-existing and postoperative intimal hyperplasia and arteriovenous fistula outcomes. Should present criteria for detecting and repairing arteriovenous fistula stenosis be reconsidered Adding entry blood move surveillance to scientific monitoring reduces thrombosis rates and prices, and improves fistula patency in the brief term: a controlled cohort research. The Society for Vascular Surgery: clinical follow pointers for the surgical placement and maintenance of arteriovenous hemodialysis entry. Can blood flow surveillance and pre-emptive restore of subclinical stenosis prolong the useful life of arteriovenous fistulae Adding access blood move surveillance reduces thrombosis and improves arteriovenous fistula patency: a randomized managed trial. Medical adjuvant treatment to improve the patency of arteriovenous fistulae and grafts: systematic evaluation and meta-analysis. Inside-out higher body venous access: the first-in-human experiences with a novel method utilizing the Surfacer inside-out access catheter system. Propensity-matched mortality comparison of incident hemodialysis and peritoneal dialysis patients. Comparison of affected person survival between hemodialysis and peritoneal dialysis among sufferers eligible for both modalities. More use of peritoneal dialysis offers important savings: a scientific evaluate and health financial decision model. Association of pre-transplant dialysis modality and post-transplant outcomes: a meta-analysis. Timing, causes, predictors and prognosis of switching from peritoneal dialysis to hemodialysis: a prospective research. Renal Association clinical follow guideline on peritoneal dialysis in adults and youngsters. Fluoroscopic guide wire manipulation of malfunctioning peritoneal dialysis catheters initially positioned by interventional radiologists.
Other groups are candidates for preemptive therapy if an acceptable monitoring system is in place and patient compliance is good blood pressure medication pills buy discount indapamide 2.5 mg. Valganciclovir and ganciclovir are associated with neutropenia; however heart attack left or right indapamide 2.5 mg discount with mastercard, dose reduction risks breakthrough viremia and the emergence of viral resistance arteria3d mayan city pack discount 1.5 mg indapamide visa. Given altering renal operate after transplantation and the prices of medicine hypertension 180120 order 1.5 mg indapamide with amex, many regimens employ decrease doses of valganciclovir. Relapse does occur, primarily in seronegative sufferers, in these with excessive viral burdens, if not treated to the achievement of a adverse quantitative assay, and in gastrointestinal disease treated with an oral routine. Repeat endoscopy could also be thought-about with poor 31 � Infection in Kidney Transplant Recipients 529 scientific response, or if different processes are current (ischemia, cancer). Such sufferers may profit from 2 to 4 months of oral valganciclovir (900 mg daily based mostly on creatinine clearance) administered as secondary prophylaxis after the completion of intravenous remedy. This approach has resulted in uncommon symptomatic relapses and has been associated uncommonly with the emergence of antiviral resistance. It may be worth measuring a formal creatinine clearance to guarantee sufficient dosing. Cidofovir may be used, however typically incurs vital nephrotoxicity and ocular toxicity. Letermovir appears to have good oral bioavailability, and a low price of opposed results and drug�drug interactions. Lymphomas constitute 15% of tumors amongst adult transplant recipients (51% in children) with mortality of 40% to 60%. Many deaths are related to allograft failure after withdrawal of immunosuppression during treatment of malignancy. In kidney transplantation, the failure to regress with vital reductions in immunosuppression may recommend the necessity to sacrifice the allograft for affected person survival. In such sufferers, the etiologies of decreased renal operate have to be carefully evaluated. Reduced immunosuppression may stabilize renal allograft operate but risks graft rejection. Reactivation occurs with immunodeficiency and immunosuppression and tissue damage. The clinical presentation of illness is often as asymptomatic, sterile pyuria, reflecting shedding of contaminated tubular and ureteric epithelial cells. These cells include sheets of virus and are detected by urine cytology as "decoy cells. If screening is carried out by plasma viral load, the interval between screening assays ought to be lowered to month-to-month for the first 6 months posttransplant. This reflects the sooner onset of permanent renal damage in patients with circulating viremia in contrast with urinary excretion. It is beneficial to monitor the response to such maneuvers using plasma viral load measurements. General targets embrace tacrolimus trough ranges of <6 ng/mL, cyclosporine trough levels <150 ng/mL, sirolimus trough ranges of <6 ng/mL, and/or mycophenolate mofetil every day dose equivalents of 1000 mg. Regardless of the strategy, renal perform (at least 1�2 times per week), drug levels, and viral hundreds (alternate weeks) should be monitored fastidiously during reductions. Significant renal toxicity could also be observed with cidofovir regardless of probenecid which may decrease efficacy. Some centers enable retransplantation after immunosuppression has been discontinued for some period. This infection could present with focal neurologic deficits or seizures and more slowly progressive neurologic lesions and will progress to dying after intensive demyelination. Prophylaxis for opportunistic infections is dependent upon the epidemiology of the individual. The drug of alternative for documented Aspergillus infection is voriconazole, despite its important interactions with calcineurin inhibitors and rapamycin. Surgical debridement is typically required for profitable clearance of such invasive infections. These infections are usually treatable by way of correction of the underlying metabolic abnormality and topical therapy with clotrimazole or nystatin (see Table 31. Optimal administration of Candida infection occurring in association with surgical drains or vascular entry catheters requires elimination of the foreign physique and systemic antifungal remedy with fluconazole or echinocandin. A single optimistic blood tradition outcome for Candida species necessitates systemic antifungal therapy; this discovering carries a significant risk of dissemination in this population. A special drawback in kidney transplant recipients is candiduria, including in asymptomatic patients. Notably in people with poor bladder function, obstructing fungal balls can develop on the ureteropelvic junction, leading to obstructive uropathy, ascending pyelonephritis, and the possibility of systemic dissemination. Aspergillus Invasive aspergillosis is a medical emergency in the transplant recipient, with the portal of entry being the lungs and sinuses in more than 90% of sufferers and the skin in a lot of the others. Brain and epidural abscesses have been observed and may be particularly problematic when secondary to an antibiotic-resistant pathogen. As famous earlier, fungi may be metastatic from lungs but also could spread from sinuses, pores and skin, and the blood. Cryptococcosis must be suspected in transplant recipients who current greater than 6 months after transplantation with unexplained headaches (especially when accompanied by fevers), decreased state of consciousness, failure to thrive, or unexplained focal skin disease (which requires biopsy for culture and pathologic evaluation). Extended courses of fluconazole suppression could also be required for patients primarily based on clinical progress or internet diploma of immunosuppression. Such reactivation can outcome in both diarrheal sickness or parasite migration with hyperinfection syndrome (characterized by hemorrhagic enterocolitis, hemorrhagic pneumonia, or both) or disseminated infection with accompanying (usually) gram-negative bacteremia or meningitis. Immigrants, refugees, vacationers to and army personnel stationed in hyperendemic regions including Africa, Asia, Latin America, and the Caribbean must be screened with Strongyloides IgG serology before transplantation and ought to be treated with ivermectin preemptively if seropositive. Pneumocystis and Fever With Pneumonitis the spectrum of potential pulmonary pathogens in the transplant recipient is broad. The depressed inflammatory response of the immunocompromised transplant patient could significantly modify or delay the appearance of a pulmonary lesion on radiograph. Focal or multifocal consolidation of acute onset is likely to be caused by micro organism. Similar multifocal lesions with subacute to persistent development are extra likely secondary to fungi, tuberculosis, or Nocardia. Additional clues can be found by inspecting pulmonary lesions for cavitation, which suggests necrotizing infection as could also be caused by fungi (Aspergillus or Mucoraceae), Nocardia, Staphylococcus, and sure gram-negative bacilli, most commonly Klebsiella pneumoniae and Pseudomonas aeruginosa. Alternative therapies are less fascinating however have been used with success, together with intravenous pentamidine, atovaquone, clindamycin with primaquine or pyrimethamine, and trimetrexate. The use of brief courses of adjunctive steroids with a gradual taper is usually helpful. Urinary Tract Infection Most urinary tract infections happen in the first yr after kidney transplant. Urinary tract an infection past 6 months after transplantation is related to reduced renal graft survival and increased mortality. The risk for vesicoureteral reflux depends in part on the surgical approach to implantation of the ureter. The main causative organisms embody gram-negative bacilli (Escherichia coli, Klebsiella, Pseudomonas, Enterobacter, Proteus) and gram-positives (largely enterococci) and fungi (Candida species). Each of these groups may manifest important antimicrobial resistance; remedy ought to be primarily based on susceptibility patterns and by the presence or absence of structural abnormalities (obstruction, delayed bladder emptying). Initial empiric remedy should embody antimicrobial agents not used previously for prophylaxis and, where potential, not utilized in prior episodes of infection given the danger for antimicrobial resistance. Upper tract illness (pyelonephritis) may require intravenous therapy initially and a 2- to 3-week whole course. Asymptomatic candiduria must be treated in sufferers with renal allografts (although data are limited) with fluconazole (200 mg orally per day for 7�14 days). Upper tract illness with Candida species suggests obstruction and requires extra intensive therapy (fluconazole four hundred mg day by day for 3�4 weeks). Few current research address whether or not the altering ecology of bacteria has lowered the efficacy of prophylaxis. Conclusions Transplant infectious disease is more and more characterised by the ability to monitor and stop an infection based mostly on prophylaxis, new antimicrobial brokers, and vaccination. Despite significant advances, infection poses a lifethreatening problem for many recipients. In the future, increased availability of pathogen-specific immune perform exams, enhanced donor and recipient screening, and a greater understanding of an infection dangers corresponding to genetic polymorphisms ought to mix with advances in transplant immunosuppression to further cut back infection dangers. Update on immunizations in strong organ transplant recipients: what clinicians have to know.
It doubtless performs an important function in facilitating cell-to-cell communication among lymphoid cells pulse pressure aortic regurgitation indapamide 2.5 mg cheap without prescription, and it has lesser effects on physiologic effector features blood pressure medication with food 2.5 mg indapamide purchase with amex. Costimulatory molecules can exert optimistic or negative influences on the effectivity of antigen presentation and recognition and alter the edge for activation of naive T lymphocytes with out having a main activating or inhibitory operate blood pressure 20090 cheap indapamide 2.5 mg on-line. The combination of anti-B7-1 and B7-2 antibodies with either cyclosporine A or sirolimus was not enough to induce long-term tolerance blood pressure zoloft generic 2.5 mg indapamide fast delivery. Many other costimulatory molecules have been investigated successfully in animal fashions, however none has yet been exploited as a goal in the clinic. It has been considered as a beautiful target for a lot of inflammatory aspects of transplantation, including depletion-associated cytokine release syndrome, ischemia-reperfusion harm, and rejection. Its predominant therapeutic impact in transplantation seems to be to limit paracrine cytokine-mediated activation throughout the graft and to mute the scientific sequelae of rejection with out altering the overall infiltrate of inciting allosensitization. It is accredited for the treatment of rheumatoid arthritis and has been more and more evaluated for a role within the remedy of graft-versus-host disease. No reports have been made from this agent in transplantation, though there are numerous trials in autoimmune indications. As mentioned beforehand, polyclonal antibodies are thought to bind to and inhibit some adhesion molecules. In that setting, the mixed regimen was overly immunosuppressive and its growth waned. In these trials, the efalizumab-based regimen was shown to facilitate preliminary engraftment and function, and to forestall islet rejection successfully. However, its use was associated with a low incidence of progressive multifocal leukoencephalopathy (approximately 1 in 10,000 exposures), which was cited as an undue threat for patients with psoriasis. Its availability for off-label use within the clinic could facilitate medical transplant trials. More just lately, it has been proven that complement, specifically that produced regionally within the kidney itself, is a contributing factor facilitating peripheral T cell maturation and rejection. It has been used in quite a few preclinical settings and proven to be effective in stopping humoral xenograft rejection in a pig-to-nonhuman-primate mannequin. Therefore therapeutic strategies for antibody-mediated rejection have recently targeted on upstream targets of the complement pathway such because the C1 advanced, which consists of C1q, C1r, and C1s, and is the primary to work together with donor-specific antibody on the endothelium. Preclinical in vitro studies have shown that blockade of C1 prevented antibody-mediated complement activation utilizing sera from sensitized patients. There are two general forms, an / kind, expressed on 95% of peripheral T cells and answerable for specifying most alloimmune responses, and a / type, involved in innate immune responses and appearing late in allograft rejection. It is efficient in mediating T cell depletion in vitro and in vivo369 and has been studied as a rescue and induction agent in renal and cardiac transplantation. T10B9 has been studied as a conditioning agent and ex vivo depletional agent for bone marrow transplantation. It has been proven to have numerous depletional and nondepletional results on human T cells. Other Experimental Antibodies and Fusion Proteins Almost all floor molecules expressed by leukocytes have been considered for therapeutic focusing on. Many have been formally investigated in early clinical trials with out enough promise to warrant further clinical improvement. Others have important promise in superior preclinical settings however have but to be examined in humans. Its major operate may be costimulatory or inhibitory, however mounting evidence suggests that it has a role in self-tolerance. Many immunotoxins are actually being investigated as tumorspecific cytotoxic agents for malignancies and have been shown to have potent antitumor results. Rhesus monkeys so handled before transplantation expertise markedly extended allograft survival with no different upkeep immunosuppression, and a big proportion survive for years after T cell repopulation. Although most of those animals finally develop continual allograft nephropathy,434 the induction effect is impressive, and it has served as the conceptual inspiration for a lot of scientific trials using T cell depletion. Modern immunosuppressive regimens must be individualized, specifically pairing induction agents based mostly on their mechanism of action to a selected scientific need, and combining them with complementary upkeep therapies. The future of transplantation continues to be cloaked by a need for extra specific therapies with broader therapeutic indices. Antibodies are extremely specific and have proven to be safe and effective drugs whose unwanted aspect effects are usually confined to the precise effects of the goal antigen certain. Although the early hopes of clinicians have been gradual to materialize, the technology related to antibody design, building, and production has consistently improved to yield a diverse array of brokers to be examined and added to the transplant armamentarium. The future is prone to see nearly exclusive use of humanized or human antibodies and fusion proteins as opposed to xenogeneic protein constructs. Past issues of antigenicity and severe cytokine launch effects are surmountable, and as a result of the focused antigens turn out to be more rationally selected based on the growing understanding of biology, the antibodies and fusion proteins are anticipated to continue to establish themselves as crucial agents not just for induction and rescue but additionally, importantly, for upkeep remedy. Trials are persevering with to discover this facet of antibody and fusion protein administration. Additionally, the use of antibody combos may become a gorgeous method of manipulating the immune response and ensuring more dependable drug supply, particularly in the context of nonadherence. Transplant clinicians will need to turn into increasingly conscious of immune therapies developed for autoimmune and malignant indications. Effect of immunosuppressive remedy for renal allografts on the number of circulating sheep red blood cells rosetting cells. Randomized scientific trial of antithymocyte globulin in cadaver renal allograft recipients: importance of T cell monitoring. Conclusion Antibodies are actually established as priceless brokers for the remedy and prevention of allograft rejection. Currently, a quantity of polyclonal and monoclonal anti-T cell antibodies have confirmed roles in the remedy of steroid-resistant acute rejection. The past 15 years have seen increasing justification for the use of antibodies as induction agents. Antibody induction has been shown to be an effective technique of reaching very low charges of acute rejection in renal 304 Kidney Transplantation: Principles and Practice 35. Immunocompetent T-cells with a memory-like phenotype are the dominant cell type following antibodymediated T-cell depletion. Molecular and useful analysis of monoclonal antibodies in help of biologics growth. Are wound problems after a kidney transplant more frequent with fashionable immunosuppression Association of the kind of induction immunosuppression with posttransplant lymphoproliferative dysfunction, graft survival, and affected person survival after major kidney transplantation. Orthotopic liver transplantation, Epstein-Barr virus, cyclosporine, and lymphoproliferative illness: a rising concern. Association of antibody induction with short- and long-term cause-specific mortality in renal transplant recipients. Dissociation of depletional induction and posttransplant lymphoproliferative illness in kidney recipients treated with alemtuzumab. Patterns of administration of antibody induction therapy and their related outcomes. Effect of oral acyclovir or ganciclovir remedy after preemptive intravenous ganciclovir remedy to forestall cytomegalovirus disease in cytomegalovirus seropositive renal and liver transplant recipients receiving antilymphocyte antibody remedy. Rapid serologic analysis of serum illness from antilymphocyte globulin remedy using enzyme immunoassay. Serum anti-rabbit and anti-horse IgG, IgA, and IgM in kidney transplant recipients. Replacing the complementaritydetermining regions in a human antibody with these from a mouse. Effect of anti-lymphocyte induction therapy on renal allograft survival: a meta-analysis. The effect of antilymphocyte induction therapy on renal allograft survival: a meta-analysis of particular person patient-level knowledge. Polyclonal and monoclonal antibodies for induction remedy in kidney transplant recipients. The role of L3T4 in T cell activation: L3T4 could also be both an Ia-binding protein and a receptor that transduces a unfavorable signal.
Results of a potential randomized study on the impact of splenectomy versus no splenectomy in renal transplant sufferers prehypertension and lupus 1.5 mg indapamide free shipping. Results of the Minnesota randomized potential trial of cyclosporine versus azathioprineantilymphocyte globulin for immunosuppression in renal allograft recipients blood pressure medication for nightmares indapamide 2.5 mg generic with amex. The late adverse impact of splenectomy on affected person survival following cadaveric renal transplantation blood pressure essentials discount 1.5 mg indapamide fast delivery. Effect of intensive plasma trade on renal transplant rejection and serum cytotoxic antibody hypertension nursing teaching generic indapamide 2.5 mg visa. Combined therapy of deoxyspergualin and plasmapheresis: a helpful treatment for antibodymediated acute rejection after kidney transplantation. The remedy of acute antibodymediated rejection in kidney transplant recipients-a systematic evaluate. A controlled trial of plasmapheresis within the therapy of renal allograft rejection. Guidelines on using therapeutic apheresis in clinical practice-evidence-based method from the Writing Committee of the American Society of Apheresis: the seventh special problem. The remark that these grafts had been accepted by each hosts led to the speculation that a phenomenon of immunologic tolerance to the pores and skin grafts was achieved secondary to "overseas" blood cells that endured in each twin as a consequence of placental fusion. The success of this process was partially because of the shortage of immunosuppression needed when an organ was transplanted between monozygotic twins. Allografts that have been attempted subsequently failed because of uncontrolled acute rejection responses mounted by the immune system. The quest to determine methods of both immunosuppression and tolerance induction in transplantation started. This functional definition is acceptable, as a outcome of multiple immunologic mechanisms along with donor and recipient elements are concerned in both inducing and maintaining tolerance to an outlined set of donor antigens in vivo. Achieving practical tolerance in transplant recipients will mandate that particular allograft-destructive responses are "switched off" while the global immune response to pathogens and carcinogens remains intact. The most robust type of transplantation tolerance thus has to be donor-specific, as opposed to mere 333 334 Kidney Transplantation: Principles and Practice immuno-incompetence, a requirement that could be examined experimentally by grafting third-party transplants and by challenging tolerant recipients to respond to virus infections and tumors. The idea of graft-specific tolerance is crucial each to preserve long-term survival of graft and host, and to get rid of the antagonistic occasions related to lifelong nonspecific immunosuppression. Elements of the innate immune system, together with macrophages, neutrophils, and complement, are activated as a consequence of tissue harm sustained throughout cell isolation or organ retrieval and ischemia reperfusion. Activation of the innate immune system inevitably results in the initiation and amplification the adaptive response that entails T cells, B cells, and antibodies. T cells require a minimum of two indicators for activation, antigen recognition (often referred to signal 1) and costimulation (referred to as signal 2). The majority of B cells require help from T cells to provoke antibody production. Antibodies reactive to donor antigens, including major and minor histocompatibility antigens and blood group antigens, can trigger or contribute to rejection early, and late, after transplantation. Multiple elements decide the decision as to how the immune response to a transplant might be triggered and evolve, including the place the antigen is "seen" and the conditions which are present at the time-in particular, the presence or absence of inflammation related to activation of the innate response. In basic, the innate response is neither particular nor is it altered significantly with a quantity of antigenic challenges. In distinction, the adaptive response is specific for a specific antigen or combination of antigens and "remembers" when it encounters the same antigen again, augmenting its activity and the rapidity of the response at each encounter. When the immune system encounters an antigen, it has to decide which kind of response to make. In most instances, despite the very fact that one element of the immune system could dominate and lead to rejection, the method is normally multifactorial, resulting from the integration of multiple mechanisms. Understanding the molecular and mobile mechanisms that lead to allograft rejection has provided insights resulting in the event of therapeutics that suppress this unwanted immune response after transplantation. A various collection of small-molecule and biologic immunosuppressive agents are permitted and obtainable to be used within the clinic which have the potential to management or inhibit allograft rejection. Each immunosuppressive agent acts on a unique side of the immune response to an allograft and can therefore be used successfully in combination. Unfortunately, all of those brokers are globally nonspecific of their suppressive exercise, and each has some deleterious unwanted aspect effects. For almost all transplant recipients, continued survival of the allograft depends on life-long administration of a number of immunosuppressive drugs. Each immunosuppressive agent targets a particular step in the activation and proliferation of T lymphocytes. The development of immunologic tolerance or specific unresponsiveness to donor alloantigens in the brief term or the long run after transplantation appears to offer the best chance of reaching effectiveness and specificity in the management of the immune system after transplantation in both the absence or a minimum of lowered a nice deal of nonspecific immunosuppressive agents. This article is subsequently devoted to dialogue of the mechanisms underlying tolerance induction and techniques used to induce unresponsiveness in transplanted allografts. The next part of the chapter units the scene for discussing the totally different approaches to tolerance induction being explored most actively at present. This leaves the T cells with receptors that have an intermediate affinity to enter the bloodstream the place they recirculate between blood and peripheral lymphoid tissue. A subpopulation of T cells that will be mentioned later, so-called thymus-derived or naturally occurring regulatory T cells (Treg), are additionally chosen in the thymus and migrate to the periphery. Second indicators or costimulation is offered by further cell floor interactions. This interaction delivers a signal to the T cell that lowers the brink for T cell activation. The two-signal mannequin of T cell activation is properly accepted, but you will want to observe that this is a simplification. Cytokines and chemokines can modulate expression of the cell surface molecules talked about previously along with the expression of cytokine and chemokine receptors themselves. Activation alerts within the form of cytokines propagate the responses initiated by signals 1 and 2 and are sometimes referred to because the third sign in T cell activation. Many experimental fashions have established that donor antigen should be present constantly to keep a tolerant state, before or after transplantation, regardless of the precise mechanisms involved. During the induction and maintenance phases of tolerance, the presence of alloantigen is the key factor driving the outcome. As is commonly the case with the immune system, the identical factor can influence the response both positively and negatively. In the case of donor antigen, presentation within the incorrect context, similar to in a proinflammatory surroundings as outlined previously, may lead to activation with the potential of destroying the tolerant state and triggering graft rejection, however once tolerance is established, persistence of antigen is crucial for maintaining the tolerant state. A constant stability exists to guarantee an efficient but not extreme response to undesirable stimuli. Many mechanisms of tolerance are, actually, continuously utilized by the body to prevent reactions towards self-antigens that may finally result in autoimmune pathologies. Many of these similar mechanisms and regulatory cell populations can be harnessed to induce and preserve tolerance to alloantigens, at least in animal fashions. The extra likely state of affairs is that completely different mechanisms work in live performance and that distinct mixtures of mechanisms are brought into play relying on donor and recipient characteristics, immunosuppression, an infection, and so forth, because the immune response to the transplant evolves. The demise or deletion of lymphocytes able to recognizing and responding to self-antigens or, after transplantation, donor alloantigens is a really effective mechanism for eliminating lymphocytes from the immune repertoire which have the potential to harm the host or the graft, thereby creating unresponsiveness or tolerance to self or donor alloantigens. Importantly, if that is the one mechanism in operation to both induce or preserve tolerance, deletion must be sustained indefinitely. Central tolerance by clonal deletion of T cells within the thymus is the major mechanism by which tolerance to self-antigens is induced. Central deletion of donor alloantigen-reactive T cells has been significantly successful within the context of therapeutic strategies utilizing donor bone marrow in combination with nonmyeloablative remedy, similar to T cell depletion or costimulation blockade, for the induction of tolerance. In blended allogeneic chimeras in the mouse, donorderived dendritic cells have been proven to reside and persist in the recipient thymus,35 leading to steady deletion of donor-reactive thymocytes resulting in the absence of donorreactive T cells within the periphery and hence tolerance to donor alloantigens. Data from some scientific research suggest that transient quite than persistent chimerism could also be sufficient in the presence of other immunosuppressive agents to achieve tolerance in some individuals,36 whereas others suggest that solely the achievement of full donor chimerism is in preserving with the ability to withdraw immunosuppression and maintain graft survival. The introduction of excessive doses of outlined antigens intravenously or orally has been shown to lead to deletion of mature T cells in the peripheral lymphoid organs. The mechanisms by which T cells are deleted in the thymus and the periphery is an area of active investigation. Two distinct modes of apoptosis have been implicated as the mechanism essential for T cell death in these settings. Fas-ligand expression has been proven to be an important contributor enabling these sites to maintain their immune privilege status.
2.5 mg indapamide discount with mastercard. Measuring Central Venous Pressure using a Patient's Arm.