
Lexapro
| Contato
Página Inicial
"Buy 20mg lexapro with mastercard, depression urban dictionary".
L. Kor-Shach, M.A., M.D., M.P.H.
Co-Director, UTHealth John P. and Katherine G. McGovern Medical School
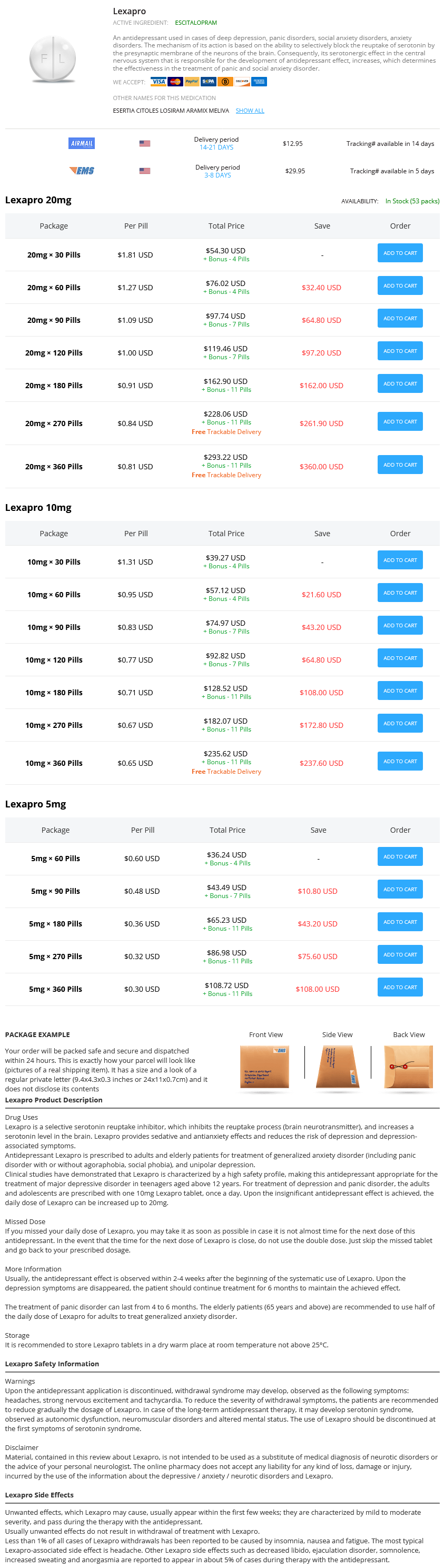
Most patients with prostatic urethral illness may have direct extension of the bladder most cancers into the prostatic urethra; however depression symptoms throwing up lexapro 10mg order fast delivery, some patients will have pagetoid spread beneath normal-appearing urothelium on the bladder neck anxiety lymph nodes lexapro 10mg purchase free shipping. Transurethral resection of the prostatic urethra is the first methodology for detecting prostatic urethral carcinoma anxiety girl meme lexapro 10mg line, with a sensitivity and specificity of higher than 90% (Wood et al mood disorder treatments buy lexapro 5mg low price, 1989a; Donat et al, 2001a, 2001b). Transurethral resection of the prostatic urethra must be performed on all sufferers with optimistic urine cytology however a negative bladder biopsy, or on those with recurrent bladder cancer after a quantity of courses of intravesical chemotherapy. The current 2009 bladder most cancers staging system now excludes noninvasive prostatic urethral illness from the T4 class. These tumors have a relatively good prognosis not consistent with T4 staging status. Only sufferers with prostatic stromal invasion, both direct or oblique, are considered to have T4a-staged disease. Transurethral biopsy of the prostate is really helpful; however, if sufferers have direct extension of the tumor via the bladder wall into the prostate, a prostate needle biopsy could additionally be warranted (Donat et al, 2001b). Patients with prostatic stromal illness are staged at T4a, and a better prognosis is associated with those who have stromal invasion by way of the prostatic urethra in contrast with invasion immediately through the bladder wall into the prostate (Esrig et al, 1996). Multimodal remedy combining chemotherapy with radical cystectomy is the appropriate therapy (Palou et al, 2007). Gene expression signatures predict outcome in non�muscle-invasive bladder carcinoma: a multicenter validation examine. Renal operate and oncologic outcomes of parenchymal sparing ureteral resection versus radical nephroureterectomy for upper tract urothelial carcinoma. Cigarette smoking and bladder most cancers in men: a pooled evaluation of 11 case-control research. The contribution of cigarette smoking to bladder cancer in girls (pooled European data). Micropapillary serous ovarian carcinoma: surgical administration and medical outcome. Risk of bladder most cancers by supply and kind of tobacco publicity: a case-control research. Risk of urinary bladder cancer amongst blacks and whites: the role of cigarette use and occupation. Tumour of the urinary bladder as an occupational illness within the rubber industry in England and Wales. Combined results of p53, p21, and pRb expression within the progression of bladder transitional cell carcinoma. Concurrent mutations of coding and regulatory sequences of the Ha-ras gene in urinary bladder carcinomas. Detection of nitrosamine production with completely different bacterial genera in persistent urinary tract infections of rats. Mediterranean dietary sample in a randomized trial: extended survival and possible reduced cancer fee. Mechanisms of prostatic stromal invasion in patients with bladder most cancers: clinical significance. The efficacy of transurethral biopsy for predicting the long-term medical impression of prostatic invasive bladder most cancers. Nodal involvement in bladder most cancers cases treated with radical cystectomy: incidence and prognosis. Haematuria investigation based on a normal protocol: emphasis on the prognosis of urological malignancy. Cancer of the urinary bladder induced in mice with metabolites of fragrant amines and tryptophan. Bladder cancer mortality in diabetics in relation to saccharin consumption and smoking habits. The sensitivity of flow cytometry in contrast with conventional cytology in the detection of superficial bladder carcinoma. Adult genitourinary sarcomas: a report of seventeen cases and evaluation of the literature. Molecular markers of urothelial most cancers and their use in the monitoring of superficial urothelial cancer. Bladder cancer stage and consequence by array-based comparative genomic hybridization. Radiation dose and second cancer risk in sufferers handled for most cancers of the cervix. The health economics of bladder most cancers: a comprehensive evaluate of the revealed literature. Drinking, micturition habits, and urine concentration as potential threat components in urinary bladder most cancers. Bladder most cancers: chemoprevention, complementary approaches and budgetary considerations. The value of the UroVysion assay for surveillance of non�muscle-invasive bladder cancer. Meta-analysis of research analyzing the connection between bladder cancer and an infection by human papillomavirus. Guideline for the administration of nonmuscle invasive bladder most cancers (stages Ta, T1, and Tis): 2007 replace. Frequent genetic alterations in simple urothelial hyperplasias of the bladder in patients with papillary urothelial carcinoma. Effect of intravesical treatment of transitional cell carcinoma with bacillus Calmette-Gu�rin and mitomycin C on urinary survivin levels and outcome. Prostatic tumor relapse in patients with superficial bladder tumors: 15-year consequence. A comparability of white-light cystoscopy and narrowband imaging cystoscopy to detect bladder tumour recurrences. Provider remedy intensity and outcomes for sufferers with early-stage bladder most cancers. Identification of chromosome 9 alterations and p53 accumulation in isolated carcinoma in situ of the urinary bladder versus carcinoma in situ associated with carcinoma. Urothelial carcinoma with an inverted development sample may be distinguished from inverted papilloma by fluorescence in situ hybridization, immunohistochemistry, and morphologic analysis. The prognostic value of E-cadherin, alpha-, beta- and gamma-catenin in bladder cancer patients who underwent radical cystectomy. Acetaminophen and the risk of renal and bladder cancer in the common follow research database. Plasmacytoid variant of bladder cancer defines patients with poor prognosis if treated with cystectomy and adjuvant cisplatin-based chemotherapy. Dietary restriction reduces insulin-like development issue I ranges, which modulates apoptosis, cell proliferation, and tumor progression in p53-deficient mice. Gene expression in the urinary bladder: a typical carcinoma in situ gene expression signature exists disregarding histopathological classification. A multivariate research of the programmed temperature vaporization injectiongas chromatographic-mass spectrometric determination of polycyclic aromatic hydrocarbons Application to marine sediments analysis. Fibroblast development issue receptor three is overexpressed in urinary tract carcinomas and modulates the neoplastic cell development. Evaluation of urinary inverted papillomas: a report of thirteen instances and literature review. Lymphovascular invasion of urothelial most cancers in matched transurethral bladder tumor resection and radical cystectomy specimens. Coffee, green tea, and caffeine consumption and subsequent threat of bladder most cancers in relation to smoking standing: a potential research in Japan. Cystectomy delay more than 3 months from initial bladder cancer diagnosis leads to decreased illness particular and overall survival. ImmunoCyt and cytokeratin 20 immunocytochemistry as adjunct markers for urine cytologic detection of bladder cancer: a potential examine. Stage pT1 bladder carcinoma: diagnostic standards, pitfalls and prognostic significance. Histologic variants of urothelial carcinoma: differential diagnosis and medical implications.
In this collection definition von depression buy generic lexapro 20mg on line, issues of the ileal conduit were compared with those of the ileocecal conduit mood disorder holistic medicine 10 mg lexapro amex, and there appeared to be no difference in the frequency of early and late postoperative problems depression symptoms diarrhea buy lexapro 5mg amex. Early issues included urinary leakage depression levels cheap 20mg lexapro with mastercard, bowel obstruction, fecal leakage, acute renal failure, fulminant hepatitis, pneumonia, gastrointestinal bleeding, hemorrhage, perforation of ileum, heart failure, and wound dehiscence. Late complications included stomal prolapse, acute pyelonephritis, bowel obstruction, urinary stones, parastomal hernia, incisional hernia, stomal stenosis, and fecal leakage. There was no difference within the incidence of decay of the higher tracts with either type of diversion. Of some notice is that at high pressures, a big portion of the ileocecal conduits experienced reflux. Whenever a portion of colon is used for a conduit, continual diarrhea may be a consequence. The segment could also be isolated on the proper or middle colic arteries, mostly the latter. The correct size of section is determined by taking into consideration the specified location of the stoma and the length of accessible ureters. The segment is isolated between bowel clamps, and a two-layer colocolostomy or stapled anastomosis is performed as outlined earlier. If a colopyelostomy is to be carried out, the phase should be placed cephalad to the bowel anastomosis. The isolated section is irrigated with copious amounts of saline till the effluent is obvious. The proximal finish is closed with a operating Connell suture of 3-0 chromic and a second layer of Lembert sutures of 3-0 silk. The ureterocolic anastomoses are then carried out (see earlier), and the tip is anchored to the retroperitoneum near the midline. The stoma is normally placed in the right higher quadrant but could additionally be positioned anyplace within the abdomen if indicated. The sigmoid colon is mobilized by incising its peritoneal attachments and the road of Toldt alongside the descending colon. The phase is isolated on the sigmoid vessels and positioned lateral to the sigmoid colon. The anastomosis of the sigmoid colon and ureterocolic anastomosis are as described for the transverse colon. IlealVesicostomy An ileal vesicostomy uses spatulated ileum and a beneficiant transverse cystotomy to decompress the bladder and to enable an appliance to be used on the abdomen. This procedure is especially nicely suited to spinal wire damage sufferers or those with significant neurologic illness. The idea is that patients with a neurogenic bladder have a neater job of caring for themselves with an abdominal stoma. The complications of the process embrace urethral incontinence requiring closure of the urethra in 20% of patients, stomal stenosis, and bladder and renal calculi. The process is performed by spatulating an ileal segment and performing a generous transverse cystotomy. The spatulated ileum is sutured to the bladder with absorbable suture, and the distal segment is brought to the abdominal wall by fashioning a rosebud stoma. All conduits are retroperitonealized, with the ureterointestinal anastomosis being positioned within the retroperitoneum. This may be accomplished by suturing the posterior peritoneum to the serosa of the conduit above the ureterointestinal anastomosis. I choose to drain the ureterointestinal anastomosis with a Jackson-Pratt or Blake closed-suction drain laid within the retroperitoneum 3 to 4 cm away from the anastomosis. For patients with extreme respiratory disease, consideration should be given to performing a gastrostomy. All patients have sequential compression boots applied as prophylaxis for pulmonary embolus. Metabolic issues are the outcomes of altered solute reabsorption by the gut of the urine that it incorporates. Many of those complications are a consequence of altered solute absorption across the intestinal section. The elements that affect the amount of solute and kind of absorption are the phase of bowel used, the surface space of the bowel, the amount of time the urine is uncovered to the bowel, the focus of solutes in the urine, the renal operate, and the pH of the fluid. Electrolyte Abnormalities Serum electrolyte complications and the kind of electrolyte abnormalities that happen are completely different, depending on the phase of bowel used. If jejunum is the phase used, hyponatremia, hyperkalemia, and metabolic acidosis happen. Other electrolyte abnormalities which were described embody hypokalemia, hypomagnesemia, hypocalcemia, hyperammonemia, and elevated blood urea nitrogen and creatinine. The metabolic alkalosis once in a while could be severe and lifethreatening (syndrome of severe metabolic alkalosis) (Table 97-10). Patients are normally efficiently handled with an H2 blocker to reduce proton secretion by the gastric segment and rehydration. In life-threatening circumstances, arginine hydrochloride infusion has been used to quickly restore acid-base balance. On occasion, when H2 blockers are ineffective, the proton pump blocker omeprazole has been efficiently used. Rarely, omeprazole is ineffective, and if the life-threatening metabolic alkalosis persists, the gastric segment must be removed (Gosalbez et al, 1993). Serum gastrin ranges are significantly correlated with systemic bicarbonate focus in gastrocystoplasty patients; the larger the gastrin level, the extra extreme the metabolic alkalosis (Tanrikut and McDougal, 2004). When quantity depletion, hypochloremia, and hypokalemia end result from vomiting in those who usually have elevated circulating gastrin levels and a persisting long-standing metabolic alkalosis, the affected person is at higher danger for improvement of the syndrome of extreme metabolic alkalosis and manifestation of the symptoms outlined beforehand. Thus, persistent lack of protons from the gastricaugmented bladder with web addition of bicarbonate to the systemic circulation, alteration of normal homeostatic mechanisms for acute adjustments in acid-base balance, and impaired capacity of even a traditional kidney to excrete bicarbonate in the face of hypochloremia, hypokalemia, and increased circulating aldosterone levels (because of the dehydration) create a vicious circle during which regular homeostatic mechanisms are circumvented. Indeed, elevated aldosterone ranges have been reported in this syndrome (Gosalbez et al, 1993). These perturbations coupled with a continued addition of bicarbonate from *Incidence as a proportion of the whole variety of reported circumstances from the literature. Finally, technical-surgical complications involve aspects of the process that end in surgical morbidity; these have been discussed after every part on the technical aspects of urinary intestinal diversion. However, at levels of serum gastrin in extra of 120ng/L, small modifications in serum gastrin levels lead to large modifications in serum bicarbonate. In view of the sigmoid correlation of serum bicarbonate to gastrin levels in patients with gastric segments within the urinary tract, patients at greatest risk for growth of the syndrome of extreme metabolic alkalosis are those whose serum gastrin concentrations exceed one hundred twenty ng/L as a result of on this portion of the curve, small additional increments in gastrin focus end in large will increase in serum bicarbonate. On the other hand, patients with serum gastrin concentrations beneath a hundred ng/L can have significant will increase in gastrin ranges with little change in serum bicarbonate. Failure to properly empty the diversion with overdistention of the gastric section could be anticipated to increase the serum gastrin stage as a outcome of stretch is a stimulus for gastrin release. For those who have either an elevated resting gastrin stage in extra of 120 ng/L or impaired renal perform, each patient and doctor must be made conscious of the consequences of dehydration and distention of the phase. Electrolyte issues that occur when jejunum is used for urinary intestinal diversion, significantly when proximal jejunum is used, include hyponatremia, hypochloremia, hyperkalemia, azotemia, and acidosis (see Table 97-10). These issues result from an increased secretion of sodium and chloride with an elevated reabsorption of potassium and hydrogen ions. This extreme lack of sodium chloride carries with it water, and thus the patient turns into dehydrated. The dehydration leads to hypovolemia, which will increase renin secretion and thereby aldosterone production (Golimbu and Morales, 1975). The excessive ranges of reninaldosterone facilitate sodium reabsorption by the kidney and potassium loss, which produce a urine low in sodium content and high in potassium. This, when presented to the jejunum, ends in a favorable concentration gradient for loss of sodium by the jejunum and elevated reabsorption of potassium, thus perpetuating the abnormalities. These electrolyte abnormalities result in lethargy, nausea, vomiting, dehydration, muscle weak spot, and elevated temperature. If the abnormalities are allowed to persist, the patient might become moribund and finally die. This syndrome may be exacerbated by administration of hyperalimentation options.
Further mobilization and separation of the posterior wall of the bladder from the anterior vaginal wall allows a tension-free closure depression quotev 10mg lexapro best. Because the trigone and ureteric orifices invariably lie in close proximity to the fistulous edges anxiety treatment centers lexapro 5mg buy generic, you will need to depression heart disease 10 mg lexapro cheap with mastercard avoid uncontrolled blunt and broad excision teenage depression symptoms quiz 10mg lexapro purchase otc, which may hamper subsequent closure. It is preferable to do a gradual and careful sharp dissection of the fistulous edges, which should be freshened. Reconstruction of vagina in two layers (arrowhead); bladder wall repaired in two layers (arrow). The closure of vagina is performed using 3-0 barbed suture, which is positioned transversely for tension-free closure as a operating watertight suture. If the size and the orientation of the vaginal gap enable less tension on the closure line, a vertically positioned suture line could probably be acceptable. The bladder is usually closed in a vertical method to reduce the contact floor of suture traces. Bladder closure is initiated at the caudal half or near the trigone space or on the most distal part of cystotomy near the ureteric orifices. If two-layer closure is contemplated, then the first layer includes mucosa and a portion of detrusor muscle layer utilizing a 4-0 monofilament absorbable suture in a working continuous trend. If the cystotomy is quite lengthy, the bladder closure could be started from the proximal open bladder edge until the superoposterior a part of the bladder is closed. Then, with new suture, the most distal segment of the cystotomy is closed until the 2 are securely knotted together roughly in the course of the cystotomy line. In so doing, the proximal suture can be utilized as traction to present higher exposure and subsequently improved visualization for the crucial a part of the cystotomy closure near the ureteric orifices. In addition, using two separate sutures for cystotomy closure avoids potential laxity of the single suture line. Tissue interposition between the bladder and vaginal suture traces is performed, preferably using a well-vascularized pedicle of omentum. To reduce rigidity on the vascular pedicle of omentum and higher mobilize this within the lower stomach, the patient is positioned in an virtually horizontal position. In case the omentum is totally retracted in the higher abdomen, it may be mobilized to start with and can be tagged to pelvis. At the anterior vaginal wall distal to the vaginal closure, a 3-0 barbed suture is positioned, which is used as a fixation to anchor the interpositional tissue. To avoid any contact between both suture strains and provide stability on fixation, the interpositional tissue is anchored with a suture on the resilient vaginal wall and distally to the end of the vaginal closure line. To prevent laxity on fixation, the interpositional tissue can be fixed left and right on the peritoneal edges of the cystotomy. Thus the interpositional tissue fully covers the suture line of the vagina, forming a triangle; every level is fastened on elastic and well-vascularized tissue. A 15-Fr Jackson-Pratt is introduced into the pelvis by way of left robotic port and secured to the skin with a silk suture. At the tip, the fascia of the 12-mm camera port is closed with monofilament absorbable suture. The drain is typically eliminated within 24 hours postoperatively or when drainage fluid is lower than 50 mL. Typically sufferers go residence inside 24 to forty eight hours with an indwelling urethral catheter, which ensures steady drainage of the bladder and proper therapeutic. Patients are warned to avoid the usage of tampons and chorus from sexual activity for a minimal of 8 weeks postoperatively. Early mobilization and ambulation are encouraged using the ideas of fast-track postoperative care: no nasogastric tube, with mobilization starting 6 hours after the top of the procedure. The patient is began on a liquid diet identical night and is progressed to a traditional food plan the subsequent day. Robotic-assisted laparoscopic restore has led to larger success charges over pure laparoscopy, which is technically harder. Major issues have been reported, including compartment syndrome in lower extremities, enterocutaneous fistula, and inferior epigastric artery injury, with the overall main complication fee being 2. Sotelo and colleagues reported an expeditious method, intentionally opening first the bladder, main accurately to the fistulous tract with out the necessity for additional vaginal incisions or further dissection of the vesicovaginal space. A few studies reported that patients were discharged with a urethral catheter and drain on the first postoperative day, whereas different facilities kept their sufferers within the hospital whereas the urethral catheter and drain were saved in place for as much as 2 weeks. Laparoscopy permits fistula repair with a limited bladder incision, not like in an open process, with all some nice advantages of minimally invasive procedures similar to a magnified view of the operative field, hemostasis, decreased hospital stay, and shorter convalescence. This series included six patients with advantages of shorter hospital stay, quicker recovery, and less morbidity. The success price reported for robotic-assisted repair was near 100 percent in most of those small sequence, with the potential benefit that the robotic device permits extra surgeons to use this minimally invasive method. Two retrospective research described transition from open to laparoscopic repair and found that the latter was minimally invasive with comparable success (Ou et al, 2004). The most significant distinction between the two teams was shorter common hospitalization (3. Ureteral catheterization is a vital step to forestall inadvertent ureteral injury during dissection as properly as throughout reconstruction. It permits visualization of the ureteric orifices inside the bladder, preventing the surgeon from taking a sew too near them during bladder reconstruction. It also keeps the working area relatively dry, and ureteral catheters could be removed on the end of the process. Such adhesions could possibly be parietal in nature, wherein adhesiolysis may be essential to allow appropriate port placement, or might be visceral whereby bowel loops might obscure the world of interest in the pelvis. Gentle and sharp dissection to assist the bowel to fall away is imperative to prevent a bowel injury throughout fistula dissection and to allow tension-free closure of the vagina and bladder. The modified technique prevents bivalving of the bladder and extensive dissection. Posterior cystotomy or limited dissection to rapidly access the fistulous web site and subsequent meticulous dissection and freshening of edges or, if needed, excision of fibrous edge are necessary. It is important to mobilize well-vascularized flaps to enable tension-free closure. If out there, omentum is preferred, especially when repairing recurrent fistula, as a result of it helps in speedy absorption of the inflammatory exudates owing to ample lymph supply, and it considerably decreases the prospect of failure. The key factors of surgery include vaginoscopy and cystoscopy to assess the fistula and placement of ureteral catheters through the fistula and normal ureters. This is achieved by placement of a ureteral catheter from the bladder, cystoscopically, cannulating the fistula and retrieving it from the vagina. Occasionally a reverse "railroading" is needed owing to the angulation of the fistulous tract, wherein the guidewire is placed transvaginally and retrieved from the bladder transurethrally. If the fistula is large, a Foley catheter could be directly positioned transvaginally into the bladder. Tugging the catheter aids in locating the approximate web site of the fistula as seen from throughout the belly cavity, allowing the position of a minimal cystotomy near the area of interest, near the midline. However, a Foley catheter positioned transvaginally by way of the fistula into the bladder permits better appreciation of the movement and site in the transperitoneal endoscopic view. Transvaginal repair stays a minimally invasive approach with little morbidity and convalescence within the palms of a talented and experienced surgeon. For patients requiring an open abdominal method or flap interposition, laparoscopic or robotic-assisted approaches offer decreased morbidity and convalescence in contrast with traditional open techniques. If obtainable, use of robotic help in laparoscopy is the popular strategy for minimally invasive surgeons. A hemostat is used to switch the fibrofatty flap from the harvest web site, by way of the tunnel, to the extent of the fistula repair. The flap is placed over the fistula repair and secured with interrupted absorbable sutures in a tension-free method. The vaginal wall flap is superior over the Martius flap and closed as previously described. A small Jackson-Pratt or Penrose drain could also be left in the labial incision within the operative mattress. The labial incision is closed, and a pressure dressing could additionally be utilized to the labial pores and skin incision. The borders of dissection embody the labiocrural fold laterally, the labia minora and the bulbocavernosus muscle medially, and Colles fascia masking the urogenital diaphragm posteriorly.
Syndromes
- Decreased blood oxygen (hypoxia)
- Mechanical -- made of man-made (synthetic) materials, such as titanium. These valves last the longest. You will need to take blood-thinning medicine, such as warfarin (Coumadin) or aspirin, for the rest of your life.
- Not sleeping very well
- Spread of Candida to other sites in your body
- Cirrhosis
- Very sore mouth with no desire to eat
The authors postulated that these sufferers might have adopted this frequent voiding preoperatively to keep away from incontinence depression for teens trusted 20 mg lexapro. Also mood disorder due to general medical condition 5 mg lexapro generic overnight delivery, growing episodes of urgency and urgency incontinence might correlate with surgical failure depression test and scale discount 5 mg lexapro otc. The causes of harm also embrace protracted obstetric deliveries depression symptoms nightmares 20 mg lexapro with mastercard, anti-incontinence surgeries, aggressive transurethral resections of the bladder neck, long-term indwelling urethral catheters, pelvic trauma, tumors, and radiation (Blaivas and Jacobs, 1991). The goals of surgical repair are to restore function and anatomy whereas fashioning an unobstructed, continent urethra (Blaivas and Heritz, 1996). Swierzewski and McGuire (1993) reviewed the records of 14 women who underwent urethral diverticulectomy throughout a 3-year period. In these sufferers important pressure was applied to the sling suspension to obtain urethral closure. Ten patients had simultaneous intestinal augmentations or diversions and a pair of had concurrent suprapubic tube placement. All of the women had been both significantly improved (12%) or cured (88%) of incontinence, and solely 2 sufferers developed de novo urgency. Rovner and Wein (2003) reported on the circumferential urethral diverticulum repair in 9 patients who obtained both end-to-end urethroplasties or dorsal urethroplasties. Flisser and Blaivas (2003) evaluated the outcomes of seventy four girls with urethral pathology who required vaginal flap reconstructions. A majority of the ladies had required reconstruction for a diverticulum or urethral fistula secondary to iatrogenic causes. The authors discovered that 73% (54) of the ladies considered themselves cured postoperatively. The presentation of sufferers with obstruction is variable and the symptoms vary from full urinary retention and urgency incontinence to the much less obvious irritative signs. Subclinical preoperative impaired detrusor contractility might manifest symptomatically with a relative obstruction when urethral resistance is increased by anti-incontinence surgery. Dysfunctional voiding or failure of rest of the exterior (striated) urethral sphincter may also have an result on emptying after surgery (Fitzgerald and Brubaker, 2001). Also, a patient who habitually voids by abdominal straining might have problem emptying after incontinence surgery. If a affected person has postoperative urethral obstruction, physical examination might reveal an irregular urethral angulation, a foreshortened nonpliable vagina, or a nonmobile urethra. Cystoscopy is helpful to rule out bladder pathology, sling perforation, and a hypersuspended urethra. However, an important criterion for a sling incision or urethrolysis remains the temporal relationship between the symptoms and the surgical process. However, a quantity of research have investigated a number of factors which may be predictive. In contrast, no affected person with a traditional detrusor contraction developed retention postoperatively. Although urodynamic research are helpful in understanding the voiding dynamics of incontinent girls, low detrusor strain and Valsalva voiding preoperatively should not exclude patients from having an anti-incontinence procedure. In this group, 28% needed extended intermittent self-catheterization (range 4 to 40 months). A key factor in assessing voiding dysfunction is the presence of prolapse that was both uncorrected at time of surgical procedure or that occurred postoperatively. Prolapse of enough measurement might kink or angulate and externally compress the urethra. After surgical procedure, apical, anterior, and posterior prolapse should be ruled out as a reason for the urethral obstruction. They concluded that concurrent surgical procedure had little adverse impact on postoperative bladder emptying. Surgical Management of Voiding Dysfunction after Pubovaginal Sling Surgery Although transient urinary retention is widespread, most patients return to spontaneous voiding within the first 10 days (Zaragoza, 1996; Cross et al, 1998b). This is done by first inserting a cystoscope into the bladder and then gently applying caudal pressure to the urethra. These outcomes might differ from short-term reduction to worsening of the urethral rigidity secondary to periurethral fibrosis (Zimmern et al, 1987; Beck et al, 1988). Transurethral resection or incision of the bladder neck is likely to fail because the sling is extraluminal and transurethral resection could trigger harm to the sphincter, injury to the bladder neck, or periurethral fibrosis, resulting in worsened incontinence or maybe a bladder neck contracture (Ghoniem and Elgamasy, 1995). After 6 weeks or when conservative measures fail, a formal urethrolysis or sling incision is indicated. Most of these series include sufferers with obstruction after completely different anti-incontinence procedures. Their conclusion was that transvaginal lateral dissection is inadequate in relieving the direct suburethral compressive drive of the sling. Petrou and colleagues (1999) reported that the suprameatal method is superior to the transvaginal approach as a end result of the previous allows entry and division of the lateral wings of the sling. In one other series of 12 girls, Petrou and Young (2002) reported decision of obstruction in 10 sufferers after retropubic urethrolysis. Carr and Webster (1997) reported complete or significant decision of symptoms in 86% of sufferers after retropubic urethrolysis. Overall, recurrent stress incontinence after formal urethrolysis is reported as 0% to 19%. Sling incision has comparable success rates (84% to 100%) and shorter operative time and less morbidity than formal urethrolysis (McLennan and Bent, 1997; Amundsen et al, 2000a; Shenassa et al, 2000; Kusuda, 2001; Nitti et al, 2002; Goldman, 2003; Thiel et al, 2005a). Ghoniem and Elgamasy (1995) had been the first to report on the profitable use of sling incision and interposition of a free graft of vaginal wall for obstruction. Shenassa and colleagues (2000) and McLennan and Bent (1997) used vaginal wall interposition in 12 and four ladies, respectively. The success charges had been 92% and one hundred pc, but stress incontinence recurred in 25% of sufferers in each sequence. Several authors have reported on successful midline or lateral sling incision with out graft interposition. In 2000, Defreitas and Herschorn (2000) had a 94% success fee in 16 ladies after lateral sling incision, with a 34% fee of recurrent stress incontinence. Lateral incision is helpful to keep away from urethral injury in cases when the sling is identified, but the dissection aircraft between the urethra and sling is difficult. In the remaining, formal urethrolysis with entrance into the retropubic area was performed. Kusuda (2001) reported successful outcomes for 5 sufferers who underwent lateral sling incision. Two of the 3 women with failure underwent subsequent profitable retropubic urethrolysis. This allowed for full launch of all retropubic house scarring that likely contributed to the failure of the suburethral sling release. Goldman (2003) carried out simple sling incision in 14 girls with iatrogenic urethral obstruction. Foster and McGuire (1993) discovered that sufferers with detrusor instability had the next fee of failure, but later research contradicted this. Carr and Webster (1997) discovered that the only parameter predictive of success was no prior urethrolysis. Recurrent obstruction could outcome from periurethral fibrosis and scarring or intrinsic harm to the urethra that has occurred from the prior urethrolysis surgery. The most common reason for failure is likely inadequate dissection and lysis of the urethra. Scarpero and colleagues (2003) reported on the value of repeat urethrolysis after failed urethrolysis in 24 women. Both transvaginal and retropubic approaches have been chosen depending on the medical state of affairs. This helps the usage of repeat urethrolysis within the face of initial failure or in instances whereby the aggressiveness of the preliminary dissection is unknown. In addition, after an aggressive transvaginal urethrolysis, a retropubic urethrolysis may also be thought of. Synthetic slings perforate 15 occasions extra usually into the urethra and are uncovered 14 occasions more typically in the vagina than autologous, allograft, and xenograft slings (Blaivas and Sandhu, 2004).
Buy generic lexapro 20 mg line. Double Jeopardy Addiction & Depression by Claudia Black PhD.