
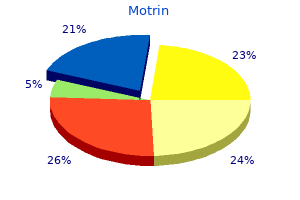
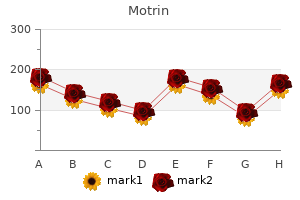
Motrin
| Contato
Página Inicial

"Motrin 400 mg order amex, pain treatment topics".
I. Campa, M.B. B.A.O., M.B.B.Ch., Ph.D.
Medical Instructor, Rocky Vista University College of Osteopathic Medicine
This permits the ulnar head to move out of the way of the rotating radius distally treatment pain base thumb buy 400 mg motrin visa. Schemitsch and Richards22 quantified the significance of the distal of the two bows in the radius pain treatment program johns hopkins buy motrin 400 mg. Restoration of this bow is the single most important step in reconstruction of the forearm after diaphyseal fracture neck pain treatment quick fix motrin 400 mg cheap without a prescription. To determine whether or not the bow has been restored after osteosynthesis pain treatment center nashville cheap motrin 600 mg on-line, draw a line from the biceps tuberosity to the sigmoid notch. At the apex of this bow on the convex aspect is the insertion of the pronator teres. The radius rotates round a longitudinal axis that passes via the center of the radial head on the proximal radioulnar joint and through the center of the ulnar head distally. Muscles and Ligaments the forearm is criss-crossed with longitudinal, oblique, and transversely directed musculotendinous units. These muscular tissues are in layers, with longitudinal muscular tissues extra superficial and crossing muscular tissues deeper. It proceeds straight down the forearm alongside the ulna border and inserts into the pisiform. Crossing the forearm in its deepest elements are a collection of obliquely oriented muscles. The supinator plays a role in each the anterior and posterior approaches to the radius. It has two heads of origin and probably may be regarded as two muscle tissue, because the fibers of every head traverse in several directions. The pronator teres originates primarily from the medial supracondylar ridge, arches obliquely across the ulnar artery and median nerve, and inserts into the apex of the bigger bow of the radius. It should be lifted from probably the most radial facet of the radius in the anterior method. It should be lifted from the radial border in an strategy to the radius and the ulna border in an strategy to the ulna. In a posterior approach to the radius, the abductor pollicis longus muscle drapes across the radius simply distal to its midpoint. The interval between the brachioradialis and flexor carpi radialis is entered, and the radial artery is retracted laterally. The supinator, pronator teres, flexor pollicis longus, and flexor digitorum superficialis could be seen. Each nerve enters the forearm from the arm in a predictable place, and each provides off key branches that must be protected. The posterior interosseous department leaves the primary nerve simply distal to the elbow and passes via the supinator muscle, between its two heads, to enter the dorsal or extensor compartment of the forearm. The course of the ulnar nerve is represented by a line drawn from the medial epicondyle to the pisiform. The median nerve enters the forearm between the brachial artery and the tendon of the biceps brachii. An isolated radius fracture typically is associated with a fall onto an outstretched hand. Matthews15 confirmed in a cadaveric study that 10 degrees of angulation of one or each bones of the forearm leads to a lack of 20 levels of pronation and supination. It is cheap to think about nonoperative remedy of an isolated ulna fracture with lower than 10 levels angulation,21 however nonoperative remedy of both-bone forearm fractures has a poor consequence. Most fractures are displaced because of the high-energy nature of the traumatic event and, subsequently, deformity is common. Patients with nondisplaced fractures normally have appreciable pain and swelling in the forearm. A systems approach to these associated accidents is as follows: Skin: Look on the pores and skin for any evidence of laceration or abrasion. Vascular: Radial and ulnar pulses distal to the site of damage should be palpated and compared to the uninjured aspect. These pulses could be troublesome to palpate because of the proximity of the fractures, so checking capillary refill in the digits is the subsequent step. For any higher extremity injury, a historical past of the causative occasion is important to perceive the diploma of vitality that the limb has needed to absorb. The patient must be questioned particularly concerning elbow or wrist pain, and neurologic symptoms of numbness, tingling, or unusual sensation in the hand. Palpation of the mid-forearm must be gentle, step by step feeling alongside the radius and ulna. Blood Supply the vascular anatomy is of important significance within the flexor compartment. Palpation must be performed of the medial and lateral epicondyles, of the scaphoid in the snuff field, and over carpal bones and the carpometacarpal joints. A systematic examination of the median, ulnar, and radial nerves involves examination of sensory and motor aspects (Table 1). The sensory examination includes static two-point discrimination of the digital nerves and lightweight touch over the autogenous zones of every nerve. On a lateral radiograph of the elbow, the radial head should align instantly with the capitellum of the distal humerus. Mino16 described a technique to interpret the lateral wrist radiograph whereby the radial styloid is aligned with the middle of the lunate, and an assessment of the overlap of the radius and ulna is made. Any shift within the ulnar head is a subluxation and, when combined with a radius fracture, represents a Galeazzi fracture-dislocation. Fractures of the radius and ulna can be considered articular fractures in the sense that functional restoration requires anatomic reduction. In the case of a displaced fracture, closed discount and forged immobilization sometimes is possible however is unreliable. The fracture with the least comminution ought to be approached first and stabilized. This allows for size to be restored in the forearm, permitting easier judgment of length within the more comminuted bone. In a stable, non-comminuted fracture, "momentary stability" may imply a plate and one screw by way of two cortices on all sides of the fracture. The plate should span the fracture complicated and provide six cortices of fixation in secure bone, each proximally and distally. Oblique fractures are treated with an interfragmentary screw or screws at right angles to the fracture line and a seven-hole plate. A unicortical locked screw could be thought-about "bicortical," but practically speaking, this rule is used only for the screw gap furthest from the fracture. In nearly all situations there should be three screw holes within the plate over secure bone away from the fracture advanced. Anterior and posterior approaches can be utilized to deal with fractures along the complete length of every bone. This location permits for wonderful soft tissue coverage, decreasing the need for plate removing. Most diaphyseal forearm fractures are finest stabilized by plates and screws, but different implants sometimes are indicated. External fixation may be used in the following settings: Open fractures with severe soft tissue injury, as a temporizing measure till reconstruction can safely be undertaken Maintenance of length in fractures with extreme bone loss (this often happens in open fractures) Patients with a number of injuries ("injury control" surgery) the Ilizarov technique is beneficial in segmental fractures, particularly when the fractures are very close to the wrist and elbow joints. A hand desk is used to rest the instruments quite than help the upper extremity. If different forearm fractures are current, however, the arm table could then be available. A non-sterile tourniquet is applied to the upper arm before prepping and draping the affected person. The surgeon normally is seated on the aspect of the hand table closest to the bone being decreased and stabilized. For a posterior or subcutaneous strategy to the ulna, the elbow is flexed, and the forearm is in a neutral place. Approach the anterior approach to the radius is the standard approach for a radius fracture, however the posterior approach is helpful when soft tissue lesions are posterior or the anterior method is compromised in some way. The arm is kidnapped to ninety degrees at the shoulder, so the whole arm lies throughout the midpoint of the hand desk. I prefer six cortices of screw fixation on either aspect of the fracture and at present use the Synthes Small Fragment Locking Compression Plates as fixation. The radial styloid and biceps tuberosity are marked, and the diathermy cord is placed between these two factors to align the incision.
Syndromes
- Stomach pain (possible bleeding in stomach and intestines)
- You have any other unexplained symptoms
- Gout
- Delirium
- Epicanthal folds, an extra fold of skin over the inner corner of the eye
- Improve height
- Excessive bleeding
It "burns no bridges prescription pain medication for uti order 400 mg motrin," and intracarpal procedures can all the time be undertaken at a later date if the radial shortening is ineffective and disease progression happens pain solutions treatment center reviews cheap 600 mg motrin fast delivery. The principle behind the use of immobilization is that by reducing the forces across the carpus backbone pain treatment yoga cheap motrin 400 mg on-line, the lunate might find a way to who pain treatment guidelines motrin 400 mg cheap overnight delivery revascularize. Consequently, the efficacy of immobilization in sufferers with stage I disease is anecdotal. The capitate should still force any fracture fragments apart, leading to collapse and displacement. While many authors have beneficial removing sufficient bone throughout radial shortening to result in an ulnar-neutral to 1-mm-positive variance,three 90% of the strain discount happens inside the first 2 mm of shortening. Circumferential subperiosteal dissection ought to be prevented to protect maximal blood supply to the osteotomy. The plate is placed over the distal radius so that its distal fixation shall be within 2 to 3 mm of the subchondral bone, with out intra-articular penetration. An oblique osteotomy has much less potential for nonunion than a transverse osteotomy1 and allows placement of an interfragmentary compression screw for added fixation. The volar locking plate is placed so that its distal fixation (represented radiographically by a Kirschner wire) travels just proximal to the subchondral floor. When utilizing a plate specifically designed for the fixation of distal radius fractures, this routinely places the osteotomy proximal to the distal radioulnar joint. A longitudinal line may be marked across the osteotomy web site to permit rotational assessment. Two to 3 mm of shortening could also be appropriate regardless of the quantity of adverse ulnar variance current. During the osteotomy, fixed cool irrigant is used to avoid thermal osteonecrosis. Final Plate Application and Osteotomy Fixation the plate and its distal fixation are then changed. Approximation of the 2 bone ends can also be facilitated by radial deviation of the wrist24 and use of a Verbrugge clamp. A bicortical screw a couple of millimeters longer than the bone width is placed 2 to 3 cm proximal to the plate and left proud. A retractor could provide the required proximal exposure without lengthening the incision. A Verbrugge clamp is positioned in the most proximal plate gap and around the proximal screw. Squeezing the clamp offers a tremendous mechanical advantage to facilitate osteotomy closure. Osteoperiosteal shingling of the volar cortex, which may facilitate osteotomy therapeutic. The Verbrugge clamp is closed manually, imparting super mechanical benefit to compress the osteotomy. If forearm rotation is limited after osteotomy, the radius must be translated radially or a lateral closing wedge part added. Use of a Verbrugge clamp compressing towards a screw proximal to the plate offers the surgeon a tremendous mechanical advantage in shortening the osteotomy. The wrist is splinted for 2 weeks, after which a detachable splint may be used and gentle motion began. The osteotomy normally heals in 2 to three months, although 4 or 5 months is often required. The exact amount of radius shortening may not be as important as the relative unloading of the lunate resulting from the shortening of the radius. Only 10 of 30 wrists had evidence of potential lunate revascularization, as indicated by decreased sclerosis and a extra normal trabecular sample. Complications were unusual; there were no nonunions, but ulnocarpal impaction developed in two patients. Lunate density was improved in 40%, unchanged in 46%, and increased (worsened) in 14%. Fifty-five p.c of wrists that underwent concurrent vascularized bone grafting of the lunate had an improved radiographic appearance, compared to only 20% that underwent isolated radius shortening. It has been suggested that prognosis is improved in younger sufferers because of elevated reworking potential. There had been no problems of radial overgrowth or development abnormalities in these sufferers. Pain, movement, and grip power had been all significantly improved after surgical procedure and the outcomes were maintained. Radius shortening was used for patients with ulnarnegative variants and closing wedge osteotomy for those with ulnar-positive variants. Iwasaki et al9 additionally famous that each radius shortening and lateral closing wedge osteotomies gave equally acceptable leads to adult sufferers. Good long-term outcomes had been reported in 100 percent of 13 sufferers at a imply of 14 years after radial closing wedge osteotomy. A second operation could sometimes be necessary for plate removal, but that is unusual. Chapter 24 Vascularized Bone Grafting and Capitate Shortening Osteotomy for Treatment of Kienb�ck Disease Nilesh M. Vascularized bone grafts from the pisiform, volar and dorsal radius metaphysis, second metacarpal head,6 and iliac crest (via free microvascular graft)2 have all been reported. Unloading procedures, like a capitate shortening osteotomy, are often combined with a revascularization process to defend the graft and to alter forces via the lunate. The dorsal metacarpal arteries lie simply deep to the fascia overlying the interossei muscular tissues. The second, third, and fourth dorsal metacarpal arteries arise from the dorsal carpal arch. It lies instantly adjacent to the posterior interosseous nerve on the radial floor of that compartment. The first and fifth dorsal metacarpal arteries are direct branches from the radial and ulnar arteries respectively. The second dorsal metacarpal artery is the preferred vascular supply for vessel implantation because of its dimension and predictable presence. Relative contraindications to vascularized grafting include: Previous surgical procedure with exposure of the dorsal side of the hand and wrist Age more than 60 years History of peripheral vascular illnesses or poorly managed diabetes Vascular grafting is accompanied by a lunate unloading procedure. Unloading has been shown to enhance signs related to Kienb�ck illness (see Chap. Altering drive distribution via the lunate serves to protect the vascular grafts and to encourage revascularization. Scaphocapitate pinning or external fixation (4 to 6 weeks) is used when ulna variance is constructive and a contraindication to capitate shortening osteotomy exists. Radius shortening and angular osteotomy is used when ulna variance is adverse (see Chap. Positioning the patient is positioned supine with the arm on a radiolucent armboard. Gravity exsanguination of the limb before tourniquet inflation allows visualization of the vessels. Approach the surgeon should think about arthroscopic evaluation earlier than the open method if the standing of the lunate articular shell is in question. Specific incision placement varies based on the graft alternative and related lunate unloading procedure. Lunate Preparation Elevate the extensor retinaculum as a radial-based flap from the fifth via the second extensor compartments to permit joint capsulotomy. The fifth extensor compartment artery is recognized and carefully traced proximally to its origin from the posterior division of the anterior interosseous artery. Enter the noncartilaginous portion of the dorsal lunate cortex using a small curette or a 2- to 3-mm round burr. Determine the graft dimension required by measuring the dorsal excavated area of the lunate.