
Rivastigimine
| Contato
Página Inicial

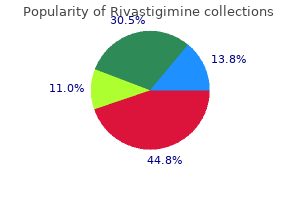
"Rivastigimine 1.5 mg generic otc, medications you can crush".
Z. Yussuf, M.B. B.CH. B.A.O., Ph.D.
Co-Director, State University of New York Downstate Medical Center College of Medicine
Once the canal is crammed with cement medicine number lookup rivastigimine 3 mg generic fast delivery, a pressurizing unit may be positioned over the proximal femur medicine 1900 order rivastigimine 6 mg with mastercard, or pressurization could be achieved with a gloved finger symptoms 5 days past ovulation order rivastigimine 6 mg visa. The prosthesis is then inserted into the doughy mass of cement with the centralizer hooked up to the tip symptoms zoloft withdrawal buy 4.5 mg rivastigimine with mastercard. The prosthesis have to be inserted with the suitable anteversion from insertion all the greatest way down. It is most well-liked to not rotate the femoral component inside the canal, as a end result of this will create undesirable cement voids. All the surplus cement is then eliminated, and the stem is held in place until the cement has fully hardened. The femoral trunion must be cleaned at this level, and the hemiarthroplasty part ought to be inserted onto the stem. The hip abductors lie over anterior hip capsule and could be damaged in an effort to get hold of sufficient exposure. The unique approach utilized by Charnley positioned the affected person in a supine position and required a trochanteric osteotomy. This strategy is used less commonly now due to issues associated with trochanteric reattachment. An incision is made within the underlying iliotibial band, after which the tensor fascia lata is retracted medially and the gluteus medius is retracted laterally. Deep dissection could require launch of the anterior components of the gluteus medius and minimus, that are raised from the femur and retracted posteriorly. The upper a half of the capsule at hip joint might be seen with mirrored head of the rectus femoris connected to the upper part of the acetabular rim. It can then be detached with greater publicity of the capsule, which can be incised. The ascending department of the lateral femoral circumflex artery and the accompanying veins run deep to the muscles and must be ligated. A longitudinal incision is made in the joint capsule, along the femoral neck and transversely from the proximal femur. A bone hook can be utilized to apply a direct lateral pressure to disimpact the femoral neck fracture. After the femur is externally rotated, adducted, and prolonged, it may be prepared. Consider detaching or splitting along the anterior third of the gluteus medius to remove the danger of damage to the superior gluteal nerve, which passes 4. Care must be taken to broach the lateral cortex of the proximal femur adequately to forestall varus malalignment of the implant. Ideal anteversion of the hip in adults is 10 to 30 degrees, dependent on multiple patient-specific elements. The presence of poor bone quality, "stovepipe" proximal femoral metaphysis and shaft, and angular/rotational deformities of the proximal femur can argue for use of a cemented implant. Proper cement approach includes vacuum mixing of cement, pressurized cement supply, proper canal preparation, placement of a cement restrictor plug, finger pressurization of cement, and secure implant pressurization of the cement. Careful retractor placement is essential to avoid errant sciatic or femoral nerve harm. Enhanced posterior capsular repair is essential to reduce the chance of dislocation. Brueton et al,6 whose radiographic analysis of 75 bipolar prostheses, had been equally divided between 32-mm and 22-mm heads, showed that the smaller head was related to extra motion. When in comparison with 9% mortality in inhabitants of similar age, the mortality after hemiarthroplasty is 10% to 40%. When an intraoperative femur fracture happens, remedy choices include methylmethacrylate combined with longstem prosthesis or, alternatively, with a totally coated cementless stem and cables. Dislocation is extra widespread with incorrect model, posterior capsulectomy, and extreme postoperative flexion or rotation with the hip adducted. Postoperative sepsis has been reported to vary from 2% to 20% and could additionally be extra frequent with the posterior surgical approach. Loosening or migration may be suspected with the presence of a radiolucent line across the prosthesis. If scientific signs and signs are present, or loosening or migration is present, a revision arthroplasty may be considered. Cementation does present some hazards, and in some circumstances the application of pressurized cement is associated with an embolization phenomenon with cement elements (ie, monomer, polymethylmethacrylate elements, or fat). The use of pulsatile lavage can scale back that risk by removing fat and marrow from the femoral canal. In older sufferers with substantial medical comorbidity, it may be clever to avoid pressurization of the cement throughout the canal, as a end result of the danger of acute embolization could also be high. These femoral prostheses have a 22- to 32-mm head that articulates with a polyethylene liner. The liner is covered with a refined metal outer shell that articulates with the acetabular cartilage. Depending on implant design, about forty five degrees of angular motion is out there before the prosthetic neck impinges on the liner and axial rotation is restricted. Theoretically, hip movement happens primarily on the prosthetic joint and only secondarily on the metal-cartilage interface. The polyethylene liner could assist to defend the native acetabular cartilage by cushioning the high-contact pressures that occur throughout the bearing. LaBelle et al14 reported no acetabular protrusio or articular cartilage wear greater than 2 mm in forty nine femoral neck fractures treated with cemented bipolar hemiarthroplasties at 5-to 10year follow-up. Wetherell and Hinves19 reported a 50% reduction in acetabular erosion for sufferers treated with a cemented bipolar prosthesis when compared to those handled with a unipolar prosthesis. Research attempting to demonstrate that motion happens inside a bipolar prosthesis has yielded conflicting outcomes. These patients with acute hip fracture proved that with regular articular cartilage, major intraoperative or intraprosthetic movement occurred in solely 25%, and most implants again functioned as unipolar. Cementless bipolar hemiarthoplasty for displaced femoral neck fractures in the aged. Effect of femoral component head dimension on movement of the two-component hemi-arthroplasty. The universal proximal femoral endoprosthesis: a short-term comparability with conventional hemiarthroplasty. Risk components influencing mortality after bipolar hemiarthroplasty within the therapy of fracture of the femoral neck. Relation to age, treatment, preoperative sickness, time of surgical procedure, and complications. Anterversion of the acetabulum and femoral neck in normals and in sufferers with osteoarthritis of the hip. Age and sex as determinants of mortality after hip fracture: 3895 patients adopted for 2. The Hastings bipolar hemiarthroplasty for subcapital fractures of the femoral neck. The femur is the lengthy bone most commonly affected, with 25% involving the proximal third of the femur. The bony construction of the acetabulum consists of the anterior and posterior columns with their respective partitions, which jut over laterally to cowl the femoral head. The anterior column is defined as the bone that extends from the iliac crest to the pubic symphysis. The posterior column starts from the articulation of the superior gluteal notch with the sacrum and extends by way of the acetabulum and ischium to the inferior pubic ramus. The acetabular dome, the superior weight-bearing region, consists of each the anterior and posterior columns and is contributed to by both walls. The principal and secondary bony trabeculations of the pinnacle, neck, and intertrochanteric space enable the pinnacle and neck arcade to face up to tremendous compressive and tensile forces. The elevated variety of immature cells, produced in response to the anemia and noted on the peripheral blood smear, is termed a leukoerythroblastic response. Hypercalcemia could additionally be seen in up to 30% of patients with extensive metastases, most commonly in myeloma, breast cancer, and non�small cell lung most cancers.
A stylus is attached to the rotational information to determine the extent on the anterior minimize medicine 93832 discount rivastigimine 6 mg line. The 4:1 slicing block is adjusted by the anterior cut floor and remaining femoral bone resections treatment urticaria cheap rivastigimine 1.5 mg overnight delivery. The tibial slicing guide is then assembled on the horseshoe information whereas the green tracker is connected medicine recall rivastigimine 1.5 mg generic with mastercard. The varus�valgus alignment medicine dropper buy rivastigimine 1.5 mg free shipping, slope, and mediolateral resection depth are displayed numerically. The navigation system merely gives accurate numerical data to assist with this decision. Computer digitization has suggested a femoral dimension based mostly on points chosen by the surgeon, however the dimension of the actual component chosen depends on many other elements that the surgeon should keep in mind when choosing the appropriate 4:1 slicing block. Tibial Rotation Tibial rotation is about using the appropriate tibial template assembled to the alignment handle and tracker. The tibial template should be aligned within the proper position, as determined by the surgeon, and pinned into the tibia. The surgeon is ready to set the depth, varus� valgus orientation, and slope of the tibial cut. Tibial rotation is set by the surgeon using the suitable tibial template and tracker. Tibial Component Insertion At this stage, osteophytes alongside the medial or lateral margins of the knee may be removed to anatomic contours. The total limb alignment and knee motion are assessed whereas trackers are connected. Soft tissue then is selectively released in accordance with the residual deformity present. However, if the surgeon prefers, the an- choring pins could be left in place throughout implantation of parts to examine for accuracy of final element place and limb alignment. The loosened tracker pin is reinserted in a secure place, and registration and anatomic survey are performed once more. It may be prevented by releasing the posterior capsule whether it is contracted, minimizing resection of the distal femur, and re-approximating the anatomic joint line. Hip heart determination Digitization Mid-range instability Position of the femoral and tibial components within the sagittal airplane have to be adjusted based on present deformity. In sufferers with hyperextension deformity: Reduce bone minimize off distal femur Place the femoral part in slight flexion In patients with flexion deformity Increase bone cut off distal femur: Avoid flexion of femoral element Tibial slope To achieve more flexion in a particular affected person, the tibial slope could also be increased barely. Decrease within the tibial slope will lead to a decreased posterior joint space and decreased flexion. Important perioperative interventions including prophylactic antibiotic, and deep vein thrombosis prophylaxis should be administered according to commonplace protocol. On the day of surgery, both passive and lively range of motion is begun, and the patient sits on the aspect of the bed, stands with help, and walks if ready. On the second and third postoperative days, the affected person transfers to and from the bed and chair, sits up in a chair, and ambulates with weight bearing as tolerated utilizing a walker or crutches. At the same time, the bodily therapist begins daily rehabilitation packages to increase knee range of movement and to strengthen the operated leg. On the third or fourth postoperative day, the affected person ought to achieve flexion of a minimal of 70 degrees and can be discharged with a walker or crutches. In the primary 2 weeks, a affected person must be visited at residence by a nurse and bodily therapist to examine the wound and proceed rehabilitation. At 2 weeks, sutures or staples are eliminated, and the affected person should be despatched to an outpatient physical remedy facility if needed. The patient is then seen on the workplace at 6 weeks and 6 months after surgery after which routinely adopted every three years. This long-term success has been related to affected person characteristics and the accuracy with which the prosthesis is implanted. The navigation system, unlike standard approach, makes it attainable to significantly improve the mechanical alignment of the limb, sagittal and frontal alignment of the femoral and tibial components, and knee vary of movement without increased short-term complications. This more correct and exact positioning and alignment of the parts should cut back the speed of long-term complications and revisions. Computer-assisted minimally invasive whole knee arthroplasty compared with normal complete knee arthroplasty: a prospective, randomized examine. Alignments and clinical ends in conventional and navigated whole knee arthroplasty. Anatomical references to assess the posterior tibial slope in total knee arthroplasty: a comparison of 5 anatomical axes. Modular femoral augments are helpful for moderate-sized bony defects, permitting the surgeon to maximize bone�prosthesis contact while restoring the joint line or posterior condylar offset. Improvements in prosthesis design and biomaterials have increased the usefulness and flexibility of steel augments in addressing larger bone defects. A systematic strategy to preoperative planning, intraoperative analysis, and reconstruction is essential in addressing femoral defects using augments. Aside from "filling the defect," it is essential to restore the femorotibial joint line and the posterior condylar offset. Significant alterations in both or each will be detrimental to the operate of the prosthesis. The joint line sometimes lies 25 mm distal to the femoral epicondyles, and the posterior femoral condyles are offset an average of 25. Cancellous bone loss necessitating cement fill, augments, or bone graft to restore cheap joint line stage. Rarely, earlier trauma resulting in extreme angular deformity might require the utilization of augments for joint reconstruction and restoration of limb alignment. Osteolytic lesions brought on by put on debris can progress and lead to loss of implant assist and eventual part loosening. Intraoperative mismanagement of defects can result in suboptimal fixation, vital alterations in knee kinematics, instability, and early implant failure. For patients with deformity, the whole size of the affected bone must be visualized. In revision cases, serial radiographs could assist assess the progression of osteolysis, radiolucent lines, and implant migration. Nuclear drugs studies together with bone scan (to detect a free prosthesis) and indium and sulfur colloid scans (to detect the presence of infection) additionally may be useful in the preoperative workup. The synovial fluid should be evaluated and cultured for the presence of microoorganisms. The particulars of the index arthroplasty with regard to ache relief and the interval to failure must be recorded. In addition, issues during the postoperative interval corresponding to falls or operative wound complications should be probed. Pain often occurs at start-up, arising from the seated place, and with stair climbing. Care is taken to drape out a large surgical field in case a more extensile strategy is critical. Preoperative Planning Thorough preoperative planning is the key to a profitable reconstruction. In all circumstances of revision, stemmed and constrained implants (or sometimes a hinged prosthesis) must be thought of and have to be out there. An intensive synovectomy and d�bridement of the medial and lateral gutters are important for decompression of the joint. In knees with severe ankylosis, techniques such because the quadriceps snip, lateral launch, and tibial turbercle osteotomy are helpful for publicity. The surgeon must know the implications of every of those releases and repair or reconstruct them correctly on the end of the procedure. The bone defect is addressed by method of cement (smaller lesions), metal augments, or structural grafts. The important points are to restore joint line, obtain acceptable alignment, and attain ligamentous balancing. Reconstruction additionally aims at restoring a secure platform for positioning and fixation of the elements. Careful preoperative planning is required to be able to handle bone loss encountered on the time of arthroplasty. Most instances of knee revision with bone loss could be addressed with the usage of a long-stem prosthesis and steel augments.
This chapter will concentrate on the remedy of a particular sample of damage to the ankle medications related to the integumentary system 1.5 mg rivastigimine order with mastercard, specifically the bimalleolar fracture sample medications in mothers milk rivastigimine 3 mg sale. The form of the tibial articular surface is concave treatment neuropathy rivastigimine 6 mg discount fast delivery, with distal extension of the anterior and posterior lips medicine to help you sleep generic rivastigimine 4.5 mg fast delivery. The anterior colliculus is the narrower and most distal portion of the medial malleolus and serves as the origin of the superficial deltoid ligaments. The intercollicular groove and the posterior colliculus, which is broader than the anterior colliculus, present the origin of the deep deltoid ligaments. The insertions of the deltoid ligaments (medial tubercle of the talus, navicular tuberosity, and sustentaculum tali) can be considered a half of the medial malleolar osteoligamentous complex. As the exterior rotation pressure continues laterally, a spiral fracture of the fibula occurs. On lateral radiograph, the fracture line will move from the anteroinferior cortex to the posterosuperior cortex. The third stage happens when the posteroinferior tibiofibular ligaments avulse or fracture off the posterior malleolus. The last stage leads to a medial malleolar osteoligamentous complicated damage with both a deep deltoid ligament tear or a fracture of the medial malleolus. Because of the pronated position of the foot at harm, however, the medial constructions are injured within the early phases. The fibula fracture pattern seen with this mechanism is often suprasyndesmotic, and the fracture pattern is an anterosuperior-to-posteroinferior fracture line as seen on the lateral radiograph. The supination�adduction sample is heralded by a low transverse fibular fracture and a vertical shearing sample medially. Finally, the pronation�abduction pattern is recognized by the avulsion of the medial malleolus and a transverse or laterally comminuted fibular fracture above the syndesmosis secondary to a direct bending second. Physical examination should middle on inspection, palpation, and neurovascular examination. If dislocation is current, the ankle must be reduced and splinted as soon as potential to forestall skin tenting and neurovascular compromise. For sufferers with a supination�external rotation pattern isolated fibula fracture who present with an intact mortise, the gravity stress examination could be revealing. More than 5 mm of medial clear area widening in association with a lateral malleolus fracture signifies an unstable sample. Pain on the ankle along the syndesmosis during a squeeze take a look at implies damage to the syndesmosis. The supination�external rotation pattern of ankle fracture is divided into four stages. Restoration of medial ankle stability is decided by the size and location of the medial malleolar fragment. In about 25% of supination�external rotation sort 4 accidents there shall be an related deep deltoid rupture. For fractures in between, an intraoperative exterior rotation stress examination ought to be carried out following malleolar fixation. Isolated lateral malleolus fractures without proof of medial-sided harm are considered supination external rotation sort 2 accidents and may be handled with useful bracing and weight bearing as tolerated. Unstable accidents ought to be treated in a well-molded shortleg cast and checked on a weekly foundation to ensure continued mortise reduction. The neurovascular anatomy in regards to the ankle must be reviewed, together with the course of the saphenous vein medially and the superficial peroneal nerve laterally. Equipment to be used features a small fragment plate and screw set, giant pelvic reduction clamps, small-diameter Kirschner wires, and three. Positioning the affected person is positioned supine with a small bump under the ipsilateral hip to ease entry to the fibula. A pneumatic tourniquet may be applied to the affected thigh if desired for use during the surgical process. The bump could also be removed after lateral fixation for easier access to the medial facet. In rare circumstances, if a posterior approach is chosen, the affected person could also be positioned in the prone position to enable entry to the posterior tibia through the posterolateral method. Direct entry to the posterior malleolus may be obtained through a posterolateral method to the fibula. Skin incision marked out simply along the posterior border of the fibula, centered concerning the degree of the fracture. Incision by way of the peroneal (lateral compartment) fascia, exposing the fracture site. Identification of the superficial peroneal nerve because it crosses proximally within the wound. Next, the peroneal fascia is divided and the peroneal tendons and musculature are retracted posteriorly. With mild elevation of the periosteum about the fracture web site, the fibula ought to be exposed. Care should be taken to keep away from extreme stripping of fracture fragments in addition to iatrogenic disruption of the syndesmotic ligaments as they insert anteriorly on the fibula. Usually reduction is afforded by a small "lion jaw" clamp or pointed reduction forceps. If discount is difficult, manual traction with pronation and external rotation will afford fracture alignment in supination�external rotation patterns. At this point, if a lateral plate is chosen, the lag screw is positioned within the anterior-to-posterior course, perpendicular to the fracture. If a posterior plate (antiglide) is chosen, the lag screw is positioned by way of the plate in a posterior-to-anterior course. Next a one-third tubular plate is placed instantly lateral on the fibula (neutralization). Fracture web site is uncovered and cleaned of hematoma and the talar dome is inspected for signs of chondral injury. After dissection of the pores and skin, the subcutaneous tissues must be fastidiously dissected to stop damage to the saphenous vein and nerve. With the dissection carried down sharply to the bone, the periosteum is elevated for 1 mm proximally and distally. The fracture should be booked open to allow visible inspection of the talar dome for chondral harm. After radiographic documentation of the discount and wire placement, cannulated screws of applicable length could also be positioned over the wires after drilling of the out cortices with a cannulated drill. Alternatively, noncannulated screws may be used independent of the provisional stabilization. If the fragment is just too small, nevertheless, one screw could suffice owing to the inherent stability of the undulating fracture line. Countersinking the screw heads medially might assist to alleviate painful distinguished hardware. The suture or wire pressure band is anchored a few more proximal screw placed parallel to the articular floor. Postreduction lateral radiograph showing a posterior malleolus fracture involving multiple third of the articular floor. Access is by way of the interval between the flexor hallucis longus and the peroneal muscle belly. If an open approach is used for discount, screws placed posterior to anterior could also be positioned throughout the fracture site. When utility of a posterior or antiglide plate is chosen, placement of a lag screw is optional. Because of the biomechanical properties of this plate assemble, this lag screw is optional. If a posterior plate is utilized, the proximal screws are placed bicortically from posterior to anterior, each proximal and distal to the fracture. The lag screw could be placed from posterior to anterior with bicortical buy achieved in every screw. Lateral displacement that enables quite a lot of millimeters of tibiofibular widening is taken into account pathologic and an indication for syndesmotic fixation.
Percutaneous intramedullary fixation of lengthy bone deformity in severe osteogenesis imperfecta symptoms 4 weeks pregnant cheap rivastigimine 3 mg online. Delayed osteotomy but not fracture therapeutic in pediatric osteogenesis imperfecta patients receiving pamidronate medicine grapefruit interaction buy cheap rivastigimine 3 mg on-line. Fragmentation symptoms 4dp5dt fet rivastigimine 4.5 mg cheap with amex, realignment medications 4 less canada purchase 3 mg rivastigimine free shipping, and intramedullary rod fixation of deformities of the lengthy bones in children. Surgical stabilization of the lower limb in osteogenesis imperfecta using the Sheffield telescopic intramedullary rod system. The extent of limb shortening and the degree of foot deformity are crucial components that decide therapy. Ideally, amputation is performed at 10�18 months of age when the kid is beginning to pull to stand. A widespread dilemma for fogeys and consulting physicians is an unwillingness to commit to a path of both multiple lengthenings or early amputation. The Syme amputation is an ankle disarticulation that preserves the heel pad as a weight-bearing surface. This procedure offers better power efficiency than a transtibial amputation, could also be self-suspending, allows weight bearing on the stump with out the use of a prosthesis, and is cartilage capped, stopping terminal overgrowth. The Boyd amputation is a modified ankle disarticulation in which the calcaneus is preserved with the heel pad and fused to the distal tibia. The greatest indications for an amputation are a large leg-length discrepancy (ie, a distinction of more than 30%) at skeletal maturity and a nonfunctional foot. The best candidate for lengthening has a smaller anticipated leg-length discrepancy (less than 10%), a steady ankle, and a fully useful foot. Because both amputation and multiple lengthenings have significant penalties, care have to be individualized. This is especially important for sufferers with leg-length discrepancies between 10% and 30%, for which both amputation and lengthening have been proven to be efficient with glorious useful outcomes. For instance, some patients with complete fibular absence have minimal leg-length inequality and foot deformity. An understanding of the anatomy of the ankle and heel is necessary to perform both the Syme or Boyd amputation process. The posterior tibial nerve and artery course posterior to the medial malleolus and break up into the medial and lateral plantar nerves. These buildings have to be protected for the heel pad to preserve its sensation and viability. Valgus alignment and stability: small angulation is accommodated through prosthetic adjustment, however bigger angulation requires correction. Ankle alignment and stability: amputation is most well-liked over lengthening when severe subluxation or instability exists. Ray deficiency (number of missing rays): amputation is indicated when the foot is nonfunctional. A scanogram and bone age should be obtained to decide the anticipated leg-length discrepancy at maturity. Epiphysiodesis may be essential to obtain this and must be deliberate appropriately. An ankle and foot series must be obtained when irregular place or motion is present on the ankle or subtalar joint or when lateral rays are absent. No genetic defect has been recognized, and no frequent teratogen is linked to fibular deficiency. Major limb malformations associated with fibular deficiency happen by the seventh week of fetal improvement. For example, if the short leg is 85% the length of the lengthy facet at age 2 years, the size of the short facet at maturity additionally will be 85% of the estimated length of the long aspect at maturity. It could require surgical treatment when prosthetic modifications are insufficient to compensate for the deformity. When amputation or lengthening is needed however should be deferred, an atypical prosthesis that accommodates the foot position can be used. Because presentation varies extensively, an examination to assess size, alignment, and performance is critical to remedy. Hip vary of motion: a typical finding is restricted internal rotation (less than 20 to 60 degrees), indicating femoral retroversion. Care ought to be taken not to go away any cartilage remnants of the calcaneus during resection. The heel pad could also be proximal to the ankle joint and could be difficult to convey distally, even after sectioning the Achilles tendon. Nonfunctional foot with hypoplastic tarsal bones, tarsal coalition, and absent rays. Because in younger kids the distal tibial physis have to be resected to acquire fusion of the calcaneus to the tibia, this is really a modification of the Boyd amputation, since distal growth of the tibia might be lost. Disadvantages Delays prosthesis becoming by several weeks while awaiting fusion Boyd Amputation Advantages Maintains most size of limb Eliminates heel pad migration Flare at the finish of the stump improves prosthetic suspension Maximizes end-bearing potential. This may be especially essential if it preserves end-bearing without a prosthesis (eg, not having to placed on a prosthesis to go from the bed to the bathroom). Preoperative Planning Syme Amputation In patients the place the tibial length at skeletal maturity is predicted to be equal to that of the alternative facet, a Boyd amputation or timed epiphysiodesis should be considered to accommodate the peak of the prosthetic foot to achieve equal limb lengths at maturity. Bowing of more than 30 degrees ought to be addressed with osteotomy on the time of amputation. They noticed that almost all youngsters stop walking around the home and not utilizing a prosthesis in early adolescence and that ideally the brief limb ought to end in the middle fifth of the shank phase of the prosthesis to optimize cosmesis and permit room for a dynamic-response foot-and-ankle unit. The tarsal bones and distal tibia epiphysis are primarily cartilaginous in infancy. If a Boyd amputation is performed early, will most likely be necessary to resect a significant portion of the superior calcaneus and distal tibia to achieve bone�bone contact for fusion. If maximum length of the tibia is a aim of remedy (eg, to permit occasional end-bearing on the stump end with no prosthesis), contemplate ready till the distal tibia epiphysis is ossified adequately to keep away from resecting the distal physis. Some authors have suggested that routine resection of the distal tibia physis should be performed. The Achilles tendon (often very tight in patients with congenital fibular absence) can be released via a separate, percutaneous incision posteriorly to enhance exposure. The plantar incision can be cut immediately right down to bone, with care to make certain that the knife blade stays perpendicular to the skin. The anterior ankle joint is opened, and the deltoid and tibiofibular ligaments are cut sharply, with care not to injure the posterior tibial nerve and artery coursing behind the medial malleolus. The foot is further plantarflexed to expose the posterior ankle joint, which is launched, exposing the posterior calcaneus and the Achilles tendon. Care is taken not to separate the calcaneal apophysis from the physique of the calcaneus. In very tight equinus, the Achilles may be launched by way of a percutaneous incision posteriorly. Once the tendon is easy to visualize, a 1-cm section of the tendon must be eliminated to stop late migration of the heel pad. The anterior incision is deepened right down to bone, again maintaining the knife perpendicular to the skin. A retractor is placed within the talus to expose the posterior capsule and Achilles tendon. Intraoperative photograph after deflation of the tourniquet, illustrating a well-perfused heel pad. Stump closure with interrupted absorbable sutures after insertion of a Steinmann pin to stabilize the heel pad. The dorsal and volar components to the fish-mouth incision meet medially and laterally simply distal to the malleoli. Sometimes the talus is small and irregularly shaped, as seen on this case, during which the L-shaped talus hooked across the back of the distal tibia. The incisions meet medially about 1 cm distal to the medial malleolus and laterally in an identical location (the lateral malleolus typically is absent in fibular deficiency).