
Rulide
| Contato
Página Inicial

"Cheap rulide 150 mg otc, 25 medications to know for nclex".
C. Ugolf, M.A.S., M.D.
Assistant Professor, Case Western Reserve University School of Medicine
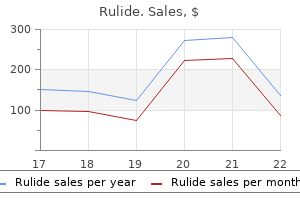
A supraglottic laryngectomy entails removing of the epiglottis medicine for pink eye rulide 150mg buy discount line, the hyoid bone medicine vs engineering 150mg rulide buy fast delivery, and the upper half of the thyroid cartilage above a airplane by way of the ventricles medicine hat alberta canada buy rulide 150mg with amex. The surface of the thyroid cartilage is exposed treatment dynamics florham park discount rulide 150mg amex, perichondrium is elevated off, and a transverse incision is made within the superior one third of the cartilage. The hypopharynx is entered through the pyriform sinus and the cut is prolonged into the vallecula. The anterior spine of the thyroid cartilage could be cut up to enhance the view of the concerned facet. Negative margins were obtained in 88% of sufferers, and disease-free survival was 91% at 1 yr. A, Antero-inferior and B, posterosuperior views of the specimen from open supraglottic laryngectomy. Note that the thyroid cartilage has been transected above the level of the glottis. Supracricoid Laryngectomy Supracricoid partial laryngectomy combines the supraglottic laryngectomy with removing of one or both vocal folds and thyroid cartilage. The operation is based on the concept that the cricoarytenoid unit is the useful anatomic unit of the larynx. As lengthy as one cricoarytenoid unit and the cricoid cartilage are left intact and functional, the operation is normally a success. Because the vocal folds are eliminated, this procedure can be carried out on motionless cords. Contraindications embrace fixation of the cricoarytenoid joint, invasion of cricoid cartilage, subglottic extension, posterior commissure involvement, and tumor extension via outer perichondrium of thyroid cartilage. This study and others highlight the crucial importance of a speech-language pathologist to maximize useful outcome. Supracricoid partial laryngectomy also has a task for salvage surgery after radiation failure in well-selected patients treated initially for T1 and T2 disease. Holsinger and colleagues reviewed 32 sufferers who underwent supracricoid partial laryngectomy for salvage and located that the rates of locoregional recurrence and disease-free interval have been much like those after total laryngectomy. In instances at high risk for thyroid invasion, similar to subglottic tumors or subglottic extension of glottic tumors, the thyroid isthmus is split and the ipsilateral thyroid gland and paratracheal nodes are taken with the specimen. After removal, the proximal trachea then is sutured to the skin to create a permanent tracheostoma. View of resected specimen from a affected person with a T3 tumor involving the preepiglottic house. The epiglottis may or may not be eliminated; removal of the epiglottis permits for the complete preepiglottic area to be resected with this process. The cricoid cartilage is left in situ with both one or both arytenoids and the related innervated musculature. View of resected specimen from a patient with a submucosal tumor of the cricoid area. Total laryngectomy contains resection of the hyoid, thyroid, and cricoid cartilages. Care have to be taken to guarantee clear margins across the tumor whereas nonetheless attempting to protect the utmost amount of pharyngeal mucosa. A full cricopharyngeal myotomy is carried out by sharply incising the muscle to enhance postoperative deglutition and alaryngeal voicing. If a nasogastric tube is to be placed, it could be accomplished at this time earlier than closing the pharynx. If planned, a tracheoesophageal prosthesis may be positioned presently by way of the posterior tracheal wall. The clavicular heads of the sternocleidomastoid are sectioned so the stoma sits more superficially, allowing simpler finger occlusion and stoma management. Options for closure of the pharynx embrace major closure, primary closure with overlay of vascularized flap, or interposition of vascularized flap. Primary closure makes use of a running inverted suture to close the pharyngeal mucosa and may be carried out in a vertical, horizontal, or T style. Vascularized flaps for interposition or overlay can be both a pectoralis major rotational flap or a free tissue transfer with radial forearm. Neck Dissection As mentioned previously, the lymphatic spread of each laryngeal subsite must be thought of to decide the need of treating the neck. The glottic larynx has poor lymphatic provide and therefore cervical metastases from isolated glottic tumors are unlikely. In distinction, the supraglottic larynx has a wealthy lymphatic supply and tends to spread to bilateral cervical lymph nodes. However, once glottic tumors grow into the supraglottis, bilateral lymphatic spread can occur. If a patient is treated with chemoradiation, nevertheless, a neck dissection should be performed for incomplete clinical response. Multimodality therapy with both surgical procedure and radiotherapy should be used for N2 or N3 illness. If conservative management fails to heal the wound, then surgical reconstruction is required, usually with the use of a vascularized tissue flap. In the late postoperative period, problems embody pharyngeal stricture, stomal stricture, and hypothyroidism. Performing a cricopharyngeal myotomy at the time of surgery improves postoperative deglutition but a stricture may still develop, leading to dysphagia and difficulty with tracheoesophageal speech. Patients might require periodic dilations of esophageal strictures in the late postoperative course. Stomal stenosis can usually be averted with proper surgical approach throughout creation of the tracheostoma, taking care to create a big stoma and obtain wound edge eversion. Hypothyroidism may end up from radiation or thyroidectomy, and due to this fact thyroid hormone ranges should be monitored frequently in the postoperative setting. Radiation Radiotherapy Planning and Techniques the logistics of radiotherapy planning and treatment are fairly detailed. Please refer to Chapter 39 for an in depth flow diagram that outlines the general logistics and therapy planning and supply paradigm. Salvage of stomal recurrence is challenging owing to the adjacent vessels and airway. The key to remedy is to forestall recurrence by sufficient protection of the peristomal tissues. Infection is treated with antibiotics and attainable opening and packing of the wound. Pharyngocutaneous fistula is a difficult complication resulting from breakdown of the pharyngeal closure whereby pharyngeal contents leak out the skin of the neck. A meta-analysis carried out by Paydarfar and colleagues32 found that preoperative radiotherapy was associated with an elevated rate of fistula formation. The major volume treated to 70 Gy is in yellow, the high-risk nodes in blue, and the low-risk nodes in pink. The entire therapy was delivered over 35 fractions, with the yellow, blue, and pink volumes treated at 2, 1. This improved precision leads to more accurate radiotherapy to tumors and fewer morbidity by sparing more normal tissue. The sagittal minimize is offered for further clarification of the dose distribution around the peristomal tissue. Morbidity Acute unwanted aspect effects include hoarseness, pores and skin irritation or burns, mucositis with dysphagia or odynophagia, dysgeusia, and xerostomia. Long-term dangers embrace laryngeal edema, dysphagia and persistent aspiration, and hypothyroidism Patients might require feeding tubes earlier than, during, and after completion of chemoradiotherapy, in addition to the occasional short-term tracheostomy before or during remedy to manage signs from the tumor and radiotherapy. As with other head and neck cancer websites, patients with advanced-stage laryngeal most cancers receiving radiotherapy require diligent nursing and supplier care during and shortly after the course of remedy to provide symptom administration and support. Chronic adjustments within the neck muscle tissue inflicting fibrosis, restricted range of neck motion, and muscle spasms can also be seen long term. Patients with at least a partial response received one more cycle of chemotherapy adopted by definitive radiation. Non-responders after two cycles of induction chemotherapy received laryngectomy adopted by postoperative radiation.
If the tumor involves the posterior maxilla and tuberosity area treatment centers for depression rulide 150mg discount line, then we prefer to make a saw cut via the Surgical Management Access the usual access for the maxilla is an upper lip break up symptoms zinc deficiency generic rulide 150 mg on line, which is straightforward and fast but has the disadvantage of leaving a midline scar medications lisinopril rulide 150 mg discount with visa. This cut may be completed with a chisel symptoms parkinsons disease discount 150 mg rulide with mastercard, and this system is beneficial to make positive the bone cuts are by way of and more probably to enable down-fracture and supply of the specimen. The subsequent a half of the operation is completion of the oral cavity incisions, which were delineated earlier and will end result in the separation of the taste bud and bone minimize through the palate from posterior to anterior. Having delivered the specimen out of the oral cavity, you will need to examine the margins of resection fastidiously and take extra tissue from areas that might be doubtful when it comes to clearance. For the low sort of maxillectomy, a fibula flap can work well, with the pores and skin island replacing the connected mucosa of the onerous palate. This type of reconstruction may give very good outcomes and may be most well-liked by the prosthodontist for implant safety, but the soft tissue interface is a drawback in comparability with bone and muscle such as the iliac crest with internal oblique. We additionally prefer this selection if the piriform and nasal bone loss is high anteriorly, as with out full assist there could be facial collapse not totally compensated by the successful dental rehabilitation. Complications Surgical issues in the immediate state of affairs embrace bleeding, airway, and aspiration in the early postoperative phase. Bleeding in the neck can occur, particularly in the intermediate section, and requires early and appropriate intervention. Flap loss, on the other hand, is less of a priority, particularly if obturation is an inexpensive choice, as the patient can recuperate and return for another try at biologic reconstruction if she or he needs. Our results1 present an involved margin and native recurrence rate of 42% and 19% for the maxilla compared to 17% and 10% for the remainder of the oral cavity cohort. Regional recurrence was reported at 26% for gingival maxillary tumors, which compared to 7% in the remainder of the oral cavity, with a conclusion that the decrease propensity for neck dissection for maxilla was resulting in poor neck management. This technique may also cover either side of the neck and avoid the necessity for bilateral neck dissection. This is been finest described in the usage of the fibula flap, with appropriate computerized preplanning and with surgery being guided with appropriate stereo lithographic slicing guides, templates, and custom-design osteosynthesis plates. Delayed Dental Rehabilitation In our unit, we favor a delayed dental rehabilitation method following reconstruction of the maxilla for malignant disease. A joint choice is made prior to surgery between the working microvascular surgeon and the maxillofacial prosthodontist regarding essentially the most appropriate free-flap reconstruction for the individual affected person, considering all the suitable factors that may contribute to the general success of the therapy approach. The dental motivation of the patient can be extremely important and contributes significantly to the decision-making course of preoperatively. Following successful surgical and oncology treatment, the patient is assessed for an implant-supported prosthesis. Prosthodontic planning is undertaken with mounted research casts and a detachable trial prosthesis the place attainable. Scans additionally reveal the presence and place of the osteosynthesis plates and whether or not this will intrude with the deliberate implant surgery. In common phrases, where no radiotherapy has been used, dental rehabilitation typically begins 4 to 6 months following treatment. If postoperative radiotherapy or chemoradiotherapy has been used, remedy is usually delayed until after the primary year posttreatment. Computerized dental implant planning software program is a superb adjunct to decide the suitable number, type, and angulation of implants into each the reconstructed bone and the native remaining bone. Implant surgery is carried out under common anesthesia, generally in a two-stage strategy with appropriate management of any intraoral skin flaps, which are debulked and tailor-made to type a vestibule wherever possible and making certain that the peri-implant tissues are motionless. The Obturated Patient In patients for whom surgical reconstruction is deemed unsuitable, the supply of a maxillary obturator is a useful different. As for all oral cancer patients, a full clinical examination of the dentition and periodontium is crucial in the provision of a successful prosthesis, particularly where retention of maxillary teeth is envisaged as part of the assist and retention for the obturator. The use of zygomatic implants compensated for the laterally placed deep circumflex iliac artery bone graft on the defect facet and the severe atrophy on the nondefect aspect. The edentulous patient is routinely treated with implants to provide retention for what otherwise would be a poor obturator prosthesis. For small unilateral posterior defects, a traditional nonimplant resolution is often well tolerated and retained. In a totally dentate individual, especially where the posterior defect only extends up to the premolar tooth on the affected aspect, a toothretained maxillary obturator with or without prosthetic tooth can provide a wonderful answer. Once the surgical defect extends into the anterior segment, our desire is to attempt the placement of zygomatic oncology implants into the affected aspect at the time of resection. Such an approach provides valuable indefect retention and support and may virtually remove any prosthesis movement in perform, which commonplace prostheses are unable to provide. The use of implants also removes the need for an ugly dental clasp on maxillary incisor teeth or the utilization of soft silicone supplies to interact undercuts throughout the defect, with their excessive maintenance requirements. The peak of the obturator element can also be saved to a minimal, which is of nice advantage to a affected person struggling with postsurgical trismus. The framework is often placed 2 weeks submit resection in a direct loading protocol. Zygomatic implant survival on this group of sufferers has been variably reported19-24 on small institutional experiences, which may represent the steep learning curve in this sort of treatment. The largest revealed sequence, by Boyes-Varley and colleagues,19 reported 100% survival on a bunch of 20 patients with forty zygomatic implants. Our own, as but unpublished, information on 102 consecutively positioned implants in 38 patients demonstrated 92% survival. Radiotherapy and Chemotherapy Radiotherapy and chemoradiotherapy for locally superior (T3/T4) tumors of the oral cavity, together with those of the maxillary alveolus, have a major role as an adjunctive therapy following doubtlessly curative surgery. For regionally superior tumors, printed sequence reporting outcomes of definitive radiotherapy alone for tumors of the maxillary alveolus indicated poor 5-year survival, although comorbidity precluding surgery and inoperability because of the extent of illness are confounding components. For smaller localized tumors (T1/T2), nonetheless, radiotherapy is a secure and effective therapy. A novel report on using an oncology zygomatic implant-retained maxillary obturator in a paediatric affected person. A definitive immediate load maxillary obturator is fitted 2 weeks following resection. Other elements embody the delivered radiation dose to the mandible and parotids, which will increase the risk of dental caries and the requirement for extractions. In the absence of great postoperative medical or surgical issues, radiotherapy ought to commence inside forty two days of surgery, as delay is understood to be detrimental to outcomes. There are significant toxicities related to radiotherapy, so advantages must outweigh the risks. Although these risks are at all times evaluated in the context of the person, revealed pointers are generally in agreement on the indications for postoperative adjuvant therapy. When evaluating a close margin, the presence or absence of perineural or lymphovascular invasion would even be considered. In these studies only 57�61% received the complete meant dose of chemotherapy; renal toxicity, thrombocytopenia, and neutropenia limited delivered doses. Intermediate-dose weekly cisplatin is being investigated within the postoperative chemoradiotherapy setting by some groups as an try and cut back toxicity while maintaining dose depth. Care must be taken to embody an adequate margin across the flap,37 the realm at high threat being the tissues across the flap somewhat than the flap itself. T4 tumors of the hard palate and maxillary alveolus have a excessive propensity for lymph node spread, and prophylactic neck dissection within the clinically node-negative neck is advised accordingly. Contralateral nodal chains should be included if the first tumor crosses or encroaches upon midline, or in the presence of great ipsilateral nodal invasion. First report of elective selective neck dissection within the management of squamous cell carcinoma of the maxillary sinus. Squamous cell carcinoma from an unknown primary website: a "selective treatment" strategy. Results of selective neck dissection in the main management of head and neck squamous cell carcinoma. Long-term results of a hundred consecutive complete neck dissections: implications for selective neck dissections. Gingival carcinoma: retrospective analysis of seventy two sufferers and indications for elective neck dissection. Cervical metastases from squamous cell carcinoma of the maxillary alveolus and hard palate. Squamous cell carcinoma of the maxillary gingival alveolus and hard palate: is there a need for elective neck dissection The utility of 3-D biomodelling expertise in complicated mandibular reconstruction-experience of forty seven scientific cases. A protocol for maxillary reconstruction following oncology resection utilizing zygomatic implants.
As a result of this flap variability medications 3 times a day safe rulide 150mg, the indications and purposes of anterolateral thigh flaps vary based on treatment tennis elbow 150mg rulide visa physique habitus medicine pacifier 150 mg rulide discount overnight delivery. The blood supply of the anterolateral thigh free flap is offered by the lateral circumflex femoral artery and vein shinee symptoms mp3 rulide 150 mg buy cheap. In 80�90% of instances, the blood supply to the anterolateral thigh free flap arises from the descending department of the lateral circumflex femoral vessels; in 10�20% of cases the blood provide to the flap arises from the transverse branch of the lateral circumflex femoral vessels. In 80�90% of circumstances, cutaneous perforators to the pores and skin paddle of the flap take a musculocutaneous course through the medial portion of the vastus lateralis muscle. The advantages of anterolateral thigh flaps arise from the relative lack of long-term donor website morbidity. However, some sufferers may experience short-term leg weak spot with some knee instability after flap harvest. Flaps wider then 8�10 cm may not close primarily and will require a pores and skin graft for closure of the thigh donor web site wound. Disadvantages of the flap come up from the thick dermis and pale skin colour of the flap, which make it a poor substitute for replacement of facial pores and skin. D, Lower extremity magnetic resonance imaging reveals bilateral congenital peroneal arteria magna, with aplasia of the posterior tibial arteries, hypoplasia of the anterior arteries, and peroneal arteries, that are the dominant blood supply to each toes, precluding use of a fibula flap. The exhausting palate was reconstructed utilizing a scapula tip bone graft that was perfused by the angular department of the thoracodorsal artery. The anterior arch of the mandible was reconstructed utilizing a serratus anterior rib myo-osseous flap component that was also perfused by the thoracodorsal artery. H, Panoramic x-ray examine 6 months after process reveals healing of the osteotomies. C, A subscapular system "megaflap" has been harvested; it incorporates a latissimus dorsi myofascial part, a serratus anterior myofascial component, and a parascapular fasciocutaneous element. D and E, the latissimus and serratus myofascial flap components have been used at the side of pores and skin grafts to reconstruct the posterior side of the defect; the parascapular flap element was used to reconstruct the anterior facet of the defect. Anterolateral thigh flaps are also the one generally used flaps for head and neck reconstruction that regularly require a musculocutaneous perforator dissection, making flap harvest barely more difficult. B, An anterolateral thigh flap is tubed for circumferential pharyngoesophageal reconstruction in this patient with a skinny physique habitus. C, the anterolateral thigh free flap has been inset and revascularized, thereby restoring pharyngoesophageal continuity. Fourteen circumstances required reexploration for impaired flap perfusion, and seven circumstances had been salvaged. Pulmonary edema and supraventricular tachycardia were the commonest medical problems occurring after free flap reconstruction. Patient comorbidity degree significantly correlated with the dangers for overall complications and medical issues, and wound-healing problems significantly correlated with a historical past of prior surgical procedure. Summary Microvascular surgical procedure has advanced considerably because the first methods have been pioneered in the Nineteen Sixties. Many of the older strategies that have been historically used for reconstruction of head and neck defects, including native and regional pedicled flaps, have been changed by free flaps that contain tissue components which would possibly be much better tailor-made for specific defects. The evolution of microvascular surgical procedure over the past a quantity of decades has been caused by the enlargement of training applications, refinement of method and equipment, and the acceptance of these flaps as a reliable and profitable reconstructive option, which has spurred their use. The excessive reliability and improved outcomes of free flaps in head and neck reconstruction deliver into question the order of reconstructive strategies within the reconstructive ladder. Complications of the pectoralis major myocutaneous flap in head and neck reconstruction. The supraclavicular artery island flap in head and neck reconstruction: applications and limitations. Analysis of outcome and complications in 400 circumstances of microvascular head and neck reconstruction. Factors associated with complications in microvascular reconstruction of head and neck defects. Salvage surgical procedure with free flap reconstruction: elements affecting consequence after therapy of recurrent head and neck squamous carcinoma. Safety of vasopressor use in head and neck microvascular reconstruction: a prospective observational research. An old controversy revisited-one versus two venous anastomoses in microvascular head and neck reconstruction using anterolateral thigh flap. Revisiting the argument for 1- versus 2-vein outflow in head and neck free tissue transfers: a evaluate of 317 microvascular reconstructions. A simplified method to the microvascular head and neck reconstruction: an 18 12 months expertise with 1500 instances. Presented to the American Academy of Otolaryngology Head and Neck Surgery Annual Meeting; Vancouver, British Columbia, Canada. Outcomes of the osteocutaneous radial forearm free flap for mandibular reconstruction. Longterm functional donor web site morbidity of the free radial forearm flap in head and neck most cancers survivors. Microsurgical reconstruction of the top and neck: interdisciplinary collaboration between head and neck surgeons and plastic surgeons in 305 cases. Prediction of outcomes in one hundred fifty sufferers having microvascular free tissue transfers to the top and neck. Internal jugular vein versus external jugular vein anastomosis: implications for successful free tissue transfer. Simplifying microvascular head and neck reconstruction: a rational approach to donor website choice. Analytic evaluation of 2372 free flap transfers for head and neck reconstruction following most cancers resection. Analysis of forty nine instances of flap compromise in 1310 free flaps for head and neck reconstruction. Prospective analysis of outcomes and complications of 300 consecutive microvascular reconstructions. Microvascular free flaps in head and neck surgical procedure: complications and consequence of a thousand flaps. The reality is that tissue engineering for practical functions in jaw reconstruction is an already established process with a simple medical methodology and a confirmed track document. In the form of in situ tissue engineering, which refers to the regeneration of bone on this case within the recipient website of the affected person, such tissue engineering represents a standard of care together with free vascular osteocutaneous flaps and autogenous cancellous marrow grafts. The Principles of Tissue Engineering In situ tissue engineering is an extension of identified bone science. That is, the regeneration and even the transforming of bone requires three components: cells, a signal, and a matrix (scaffold). The trocar, sheath, and inner barrel of two 20-mL syringes are coated with a heparin-saline answer of 2,000 models of heparin per milliliter. Although comparable and maybe even identical cells could reside in adipose tissue, these used for bone regeneration today are derived from bone marrow via aspiration. This composite graft completes the tissue engineering triangle and takes far much less time and has far much less morbidity than an open bone harvest required for a cancellous marrow graft or the harvest of a free vascular osteocutaneous graft. The canisters the tissue bed that results from a benign tumor resection has not been compromised by radiation or continual infection. Therefore, such grafts are positioned as an instantaneous reconstruction often with preservation of the neurovascular bundle. The authors stabilize the defect with a titanium reconstruction plate utilizing four bicortical locking screws in every segment. The particulate nature of an in situ tissue-engineered graft is contained by a titanium mesh on the inferior border. Defects within the Maxilla in a Non-radiated Tissue Bed the dissection of the tissue bed in the maxilla must avoid a communication into the nasal cavity and should undermine the labial mucosa sufficiently to obtain a tension-free closure. The graft materials is compacted into the mesh earlier than placement utilizing the rule of thumb of 0. Such grafts can stand up to tissue borne prosthesis because of the protective quality of a inflexible mesh. In situ tissue-engineered grafts within the maxilla require 6 months for maturity, at which era the mesh is removed and dental implants with the right trajectory for an equipment coordinated to the mandibular arch can be positioned. Continuity Defects of the Mandible from Gunshot Wounds or Infections In most instances of continuity defects of the mandible from gunshot wounds or an infection, the identical software of an in situ tissue-engineered graft is used. However, in cases of serious delicate tissue loss of both pores and skin or mucosa, a free fasciocutaneous flap, similar to a radial forearm or anterior lateral thigh flap, is required.
Intraoperative navigation in the maxillofacial area based mostly on 3D imaging obtained by a cone-beam gadget treatment hepatitis c 150 mg rulide order fast delivery. Intraoperative conebeam computed tomography in oral and maxillofacial surgical procedure using a C-arm prototype: first scientific experiences after remedy of zygomaticomaxillary complex fractures treatment with chemicals or drugs 150mg rulide. Clinical indications and views for intraoperative cone-beam computed tomography in oral and maxillofacial surgery medications known to cause pancreatitis rulide 150 mg buy cheap on line. Intraoperative laparoscope augmentation for port placement and resection planning in minimally invasive liver resection medicine rheumatoid arthritis purchase rulide 150 mg otc. Augmented reality: a new tool to enhance surgical accuracy throughout laparoscopic partial nephrectomy Radiologically assisted navigation in cochlear implantation for X-linked deafness malformation. Target quantity definition for exterior beam partial breast radiotherapy: scientific, pathological and technical studies informing current approaches. Virtual 3D tumor marking-exact intraoperative coordinate mapping improve post-operative radiotherapy. Patterns of Nodal Metastasis by Site of Primary Tumor the lymph nodes in the neck are categorised primarily based on a modification of the unique Memorial Sloan Kettering Cancer Center classification adopted by the American Head and Neck Society and Committee for Head and Neck Surgery and Oncology of the American Academy of Otolaryngology�Head and Neck Surgery. The lymph nodes in the neck are subdivided into particular anatomic subsites and are grouped into seven levels2 (Table 9. Some of the earliest experiments that led to understanding of the patterns of lymph node drainage within the neck have been carried out by Ugo Fisch in the Nineteen Sixties. He injected oil-based distinction media into the postauricular lymphatics, and the drainage pathway was studied using lymphography. Contrast flowed from these junctional nodes to nodes along the spinal accent nerve posteriorly and alongside the jugular nodes anteriorly. Understanding the patterns of lymph node metastasis is essential in figuring out the lymph node teams at highest danger for metastasis from a major tumor. This understanding of the orderly and predictable spread allows us to deal with the lymph node groups which would possibly be at highest threat for disease whereas minimizing morbidity by pointless dissection of lymph node teams at low danger. Work by Shah and Lindberg1,7 helped to map the lymph node ranges most at risk based on location of the first tumor websites. Neck dissection carries significant morbidity, with up to 70% of sufferers complaining of shoulder pain and 33% having important neck ache after surgery. In the literature, occult nodal metastases occur in 26�33% of head and neck cancer sufferers. For oral cavity cancers, a third option of using sentinel lymph node biopsy in chosen cases12,thirteen exists, and that is mentioned within the second part of this chapter. The choice to carry out an elective neck dissection is guided by an evaluation of the danger of occult metastasis to the nodal basin. Weiss and colleagues carried out a call tree evaluation and concluded that sufferers could possibly be safely observed if the likelihood of occult cervical metastasis was lower than 20%; if the danger was greater than 20%, elective treatment of the neck was warranted. Oral Cavity Other than sentinel lymph node biopsy, depth of invasion by the primary tumor is presently one of the best predictor of occult nodal metastasis. Close surveillance of the neck is an affordable strategy for tumors the place the depth of invasion is 2 mm or less, provided that the rate of lymph node metastasis is extremely low. The Brazilian Head and Neck Cancer Group performed a multicenter potential trial evaluating the efficacy for elective supraomohyoid neck dissection to modified radical neck dissections Larynx the varied subsites of the larynx have totally different lymphatic drainage patterns, and this has important implications for remedy. The supraglottis drains bilaterally into lymphatics alongside the superior laryngeal artery and drains into the jugular chain of nodes. The subglottis drains into lymphatics that travel alongside the inferior thyroid artery and into the pretracheal lymph nodes. Elective Neck Irradiation Performing a neck dissection carries the good factor about extra correct nodal staging as properly as avoidance of the short-term and long-term unwanted side effects of radiation remedy. Elective neck irradiation, however, gives lymph node failure rates of less than 5% when the first lesion was adequately managed. Practically speaking, this often means finding enlarged nodes on both bodily examination or imaging research, or a optimistic biopsy end result. Moreover, previous to the advent of radiation therapy, radical surgical resection represented the only available remedy possibility and likelihood for remedy. In maintaining with the established principles of surgical oncology, the earliest pioneers of neck dissection described and championed en bloc extirpation of all cervical nodal teams from the mandible to the upper clavicle. This philosophy remained popular throughout the early to mid-20th century, as the surgical management of head and neck cancer in many ways mirrored the evolution of surgical most cancers remedy as a whole. In addition to elimination of disease, the surgeon must also be extremely cognizant of the functional impacts of a given operation and should balance the need for efficient oncologic treatment with minimizing undue surgical morbidity. Since the original description of the unconventional neck dissection by Crile in 1906,24 there has been a gentle evolution towards extra focused and fewer radical procedures. This has been due in giant part to increased awareness and appreciation for the postoperative morbidity related to radical en bloc resections. Over time, more selective procedures targeting particular at-risk nodal basins have turn out to be more widely used, especially in clinically negative necks or in instances of restricted nodal burden. Contemporary thought has now challenged this dogma and demonstrated the utility and efficacy of more selective surgery even in sufferers with gross nodal illness. In general phrases, neck dissection is carried out in three clinical eventualities: elective neck dissection, which is carried out on the time of the primary surgery in sufferers with out clinically evident nodal disease; therapeutic neck dissection, which is performed in patients with known nodal illness; and as a salvage procedure following definitive radiation or chemoradiation remedy. In the case of elective surgical procedure for N0 disease, the safety and efficacy of selective neck dissection has been nicely established. Although it will seem intuitive to presume that disease will always be current in clinically constructive nodes. Similar findings were reported by Byers,33 who confirmed an general recurrence price of around 6% following practical node dissection with using appropriately selected adjuvant radiation. Similar findings were reported in a 10-year retrospective evaluate by Andersen and colleagues. It ought to be famous that, as with most of the previous research, the majority of patients obtained adjuvant radiation therapy, and the authors stressed the importance of prudent patient choice. Based on the outcomes of these and different studies, there would seem to be an expanded function for selective node dissection in treatment of the node-positive neck. Whatever method is to be used, a comprehensive physical examination and review of diagnostic research are essential requirements in order to provide one of the best surgery for a specific affected person. Moreover, the top and neck surgeon must be able to adapt the surgical plan intraoperatively as dictated by the appearance, habits, and burden of the disease, so as to present the most effective oncologic end result with the lowest potential threat of recurrence. As a outcome, surgical intervention including neck dissection is often used for salvage therapy following chemoradiation. The role and performance of neck dissection after definitive radiation with or without chemotherapy is likely one of the less studied makes use of of this operation. In common, neck dissection can be utilized in two scientific scenarios: the first contains neck dissection after chemoradiation with none evidence of persistent or recurrent illness in the neck; and the second entails surgical procedure for persistent and/or recurrent disease following chemoradiation therapy. Although the surgical rules are related, salvage neck dissection is a novel operation with its personal specific issues. The first concern is the relative unreliability of conventional imaging and diagnostic tools in assessing the neck following radiation and chemoradiation. In fact, only 39�46% of patients deemed to have incomplete scientific response had been found to have residual disease following salvage neck dissection throughout several series. Another necessary consideration in the decision to carry out salvage neck surgical procedure is the elevated fee of postoperative problems and morbidity. Many surgeons choose to carry out reconstruction with rotational myocutaneous flaps in these settings, particularly if the main neck vasculature is in danger because of sacrifice of overlying soft tissue. A last necessary consideration when committing to carry out post-treatment salvage neck dissection is figuring out the extent of surgery. The key elements that influence this dedication are the stage of the neck previous to therapy in addition to the clinical and imaging evaluation before and after remedy. However, the administration of sufferers with N2-N3 disease remains controversial, particularly in circumstances of fine therapy response. Based on several prior research, Pellitteri and colleagues in 2006 really helpful deliberate neck dissection for patients with N2-N3 disease no matter obvious clinical response. However, a latest prospective, randomized trial reported by Mehanna and associates calls into query the need for deliberate, post-treatment neck dissection for all cases of advanced nodal disease. The rationale for performing extra selective surgical procedure even in salvage instances is predicated on developments in radiation methods, extra accurate imaging know-how, and the improved response to chemoradiation seen with p16+ disease. Moreover, a more restrained surgical strategy can also be supported by emerging medical evidence. Several research have proven selective salvage neck dissection to be an effective approach in a majority of cases with a low danger of subsequent neck failure.
Cheap rulide 150 mg mastercard. From a Loved One's Perspective: Depression (Common Symptom of MS).