
Stromectol
| Contato
Página Inicial

"Discount 3 mg stromectol fast delivery, antibiotic impetigo".
R. Giores, M.B. B.CH. B.A.O., M.B.B.Ch., Ph.D.
Professor, Center for Allied Health Nursing Education
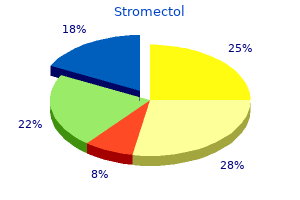
The bilateral spastic paralysis is produced by the chopping of the descending tracts apart from the corticospinal tracts antibiotics for ear infection stromectol 6 mg buy generic online. In bilateral loss of all sensations below the level of the lesion antibiotics for dogs eye discount stromectol 12 mg line, lack of tactile discrimination and vibratory and proprioceptive sensations is as a outcome of of antibiotic 10 days discount 6 mg stromectol with visa bilateral destruction of the ascending tracts in the posterior white columns bacteria 1 infection stromectol 6 mg cheap without prescription. The loss of ache, temperature, and lightweight touch sensations is caused by section of the lateral and anterior spinothalamic tracts on both sides. Because these tracts cross obliquely, the loss of thermal and lightweight contact sensations occurs two or three segments below the lesion distally. The wire is pressed on anteriorly by the vertebral our bodies and posteriorly by the bulging of the ligamentum flavum, causing injury to the central area of the spinal cord. Radiographs of those accidents typically appear normal as a end result of no fracture or dislocation has occurred. The following characteristic clinical options are seen after the interval of spinal shock has ended: 1. Bilateral decrease motor neuron paralysis within the phase of the lesion and muscular atrophy is caused by injury to the neurons within the anterior grey columns. In bilateral spastic paralysis under the level of the lesion with attribute sacral "sparing," lower limb fibers are affected lower than higher limb fibers as a end result of the descending fibers in the lateral corticospinal tracts are laminated, with the higher limb fibers situated medially and the lower limb fibers located laterally. In bilateral loss of pain, temperature, gentle touch, and pressure sensations under the level of the lesion with characteristic sacral "sparing," because the ascending fibers in the lateral and anterior spinothalamic tracts are additionally laminated, with the upper limb fibers located medially and the decrease limb fibers positioned laterally, the upper limb fibers are more prone to injury than the decrease limb fibers. Thus, the scientific image of a patient with a history of a hyperextension harm of the neck, presenting with motor and sensory tract injuries involving principally the higher limb, would strongly recommend central twine syndrome. The sparing of the lower part of the body could also be evidenced by (1) the presence of perianal sensation, (2) good anal sphincter tone, and (3) the flexibility to transfer the toes barely. In patients whose harm is brought on by edema of the spinal twine alone, the prognosis is often superb. Here, once more, as a end result of Hemisection of the spinal wire could be caused by fracture dislocation of the vertebral column, by a bullet or stab wound, or by an increasing tumor. The following attribute scientific features are seen in patients with full hemisection of the twine. Ipsilateral lower motor neuron paralysis within the phase of the lesion and muscular atrophy are attributable to damage to the neurons on the anterior grey column and probably by damage to the nerve roots of the same segment. The contralateral lack of tactile sense is incomplete as a result of discriminative touch traveling within the ascending tracts in the contralateral posterior white column remains intact. In ipsilateral spastic paralysis under the extent of the lesion, an ipsilateral Babinski signal is present, and, relying on the section of the twine damaged, an ipsilateral loss of the superficial belly reflexes and cremasteric reflex happens. All these indicators are because of lack of the corticospinal tracts on the side of the lesion. Spastic paralysis is produced by interruption of the descending tracts apart from the corticospinal tracts. Ipsilateral band of cutaneous anesthesia in the segment of the lesion outcomes from destruction of the posterior root and its entrance into the spinal twine at the stage of the lesion. Ipsilateral lack of tactile discrimination and of vibratory and proprioceptive sensations below the level of the lesion are attributable to destruction of the ascending tracts in the posterior white column on the same aspect of the lesion. Contralateral lack of ache and temperature sensations below the extent of the lesion is due to destruction of the crossed lateral spinothalamic tracts on the identical side of the lesion. Because the tracts cross obliquely, the sensory loss occurs two or three segments under the lesion distally. Contralateral but not full lack of tactile sensation beneath the extent of the lesion situation is brought on Syringomyelia, which is due to a developmental abnormality within the formation of the central canal, most often impacts the brainstem and cervical area of the spinal wire. At the location of the lesion, cavitation and gliosis in the central area of the neuroaxis occurs. Pain and temperature sensations are lost in dermatomes on both sides of the physique related to the affected segments of the wire. This loss generally has a shawllike distribution brought on by the interruption of the lateral spinothalamic tracts as they cross the midline in the anterior gray and white commissures. Tactile discrimination, vibratory sense, and proprioceptive sense are regular as a result of the ascending tracts within the posterior white column are unaffected. As the lesion expands within the lower cervical and upper thoracic area, it destroys the anterior horn cells of these segments. Bilateral spastic paralysis of both legs could occur, with exaggerated deep tendon reflexes and the presence of a positive Babinski response. These indicators are produced by the additional enlargement of the lesion laterally into the white column to involve the descending tracts. Although myelin is comparatively wealthy in lipid (70% to 80%), it additionally contains proteins that play a role in myelin compaction. Mutations in the construction of myelin protein can possibly occur and be answerable for some inherited types of demyelination. Because of the widespread involvement of different tracts at different levels of the neuroaxis, the indicators and signs are a quantity of, however remissions do happen. Ataxia because of involvement of the tracts of the cerebellum may happen, but spastic paralysis can also be present. Recent analysis has advised that the remissions in a quantity of sclerosis could in part be explained by the transforming of the demyelinated axonal plasma membrane in order that it acquires a higher than regular variety of sodium channels, which permit conduction of motion potentials despite the lack of myelin. This is brought on by the interruption of the descending autonomic fibers in the reticulospinal tracts within the lateral white column by the increasing lesion. Poliomyelitis is an acute viral an infection of the neurons of the anterior grey columns of the spinal cord. Immunization has tremendously lowered the incidence of poliomyelitis, which was as quickly as a feared disease. In severe poliomyelitis, respiration could also be threatened because of the paralysis spreading to the intercostal muscle tissue and diaphragm. Improvement usually begins at the end of the primary week as the edema in the affected area subsides, Amyotrophic lateral sclerosis (Lou Gehrig disease) is a illness confined to the corticospinal tracts and the motor neurons of the anterior gray columns of the spinal twine. Amyotrophic lateral sclerosis is a persistent progressive disease of unknown etiology. The lower motor neuron indicators of progressive muscular atrophy, paresis, and fasciculations are superimposed on the indicators and symptoms of higher motor neuron disease with paresis, spasticity, and Babinski response. Autoimmunity, infection, and heredity, alone or together, may play a task in its etiology. The degeneration of the inhibitory nigrostriate fibers ends in a reduction in the release of the neurotransmitter dopamine throughout the corpus striatum. This results in hypersensitivity of the dopamine receptors in the postsynaptic neurons within the corpus striatum, which become overactive. The characteristic indicators of the illness embody tremor and cogwheel rigidity (hyperkinetic activity) and issue initiating voluntary actions, which are slow (hypokinetic activity). Pernicious Anemia Pernicious anemia, a type of megaloblastic anemia, is caused by vitamin 1312 deficiency. Widespread sensory and motor losses could also be present because of involvement of the ascending and descending tracts of the spinal twine. Vertebral Column Radiography the views commonly utilized in radiography are anteroposte- rior, lateral, and indirect. Vertebral destruction due to tuber- culosis or primary or secondary tumors of the vertebrae or fractures because of trauma usually can be revealed by radiographic examination. Erosion of the pedicles by a tumor within the intervertebral foramina could additionally be seen. Narrowing of the area between the vertebral our bodies with bony spurs due to osteoarthritic adjustments in adjoining vertebral bodies can be seen. A protrusion of an intervertebral disc may be identified, and the presence of narrowing of the vertebral canal (spinal stenosis) can be diagnosed. The elements of a vertebra, the intervertebral the subarachnoid space may be studied radiographically by the injection of a distinction medium into the subarachnoid area by spinal tap. If the affected person is sitting within the upright place, the oil sinks to the decrease restrict of the subarachnoid house on the level of the lower border of the second sacral vertebra. By putting the patient on a tilting table, the oil can be made to gravitate steadily to larger ranges of the vertebral column. A normal myelogram will show pointed lateral projections at common intervals at the intervertebral space ranges as a outcome of the opaque medium fills the lateral extensions of the subarachnoid area around every spinal nerve. The presence of a tumor or a prolapsed intervertebral disc could impede the movement of the oil from one area to another when the affected person is tilted. The spinal cord is composed of an internal core of grey matter surrounded by an outer covering of white matter.
Artemisia Annua (Sweet Annie). Stromectol.
- Dosing considerations for Sweet Annie.
- What is Sweet Annie?
- Malaria, AIDS-related infections, anorexia, arthritis, bacterial and fungal infections, bruises, common cold, constipation, diarrhea, fever, gallbladder disorders, indigestion, jaundice, night-sweats, painful menstruation, psoriasis, scabies, sprains, tuberculosis, and other conditions.
- Are there safety concerns?
- How does Sweet Annie work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96738
Match the numbers listed below on the left with the suitable lettered construction listed on the right antibiotics for uti cipro dosage stromectol 3 mg cheap amex. The head of the caudate nucleus is connected to the putamen of the lentiform nucleus vyrus 986 m2 kit generic 3 mg stromectol with visa. The head of the caudate nucleus lies lateral to the anterior horn of the lateral ventricle antibiotic resistance wildlife stromectol 3 mg generic. Each a part of the cerebral cortex is projected to particular elements of the corpus striatum antibiotic resistance cattle order stromectol 12 mg free shipping. Glutamate is the neurotransmitter at the nerve endings of the corticostriate fibers to the corpus striatum. The largest enter to the completely different elements of the corpus striatum is from the sensory motor a part of the cerebral cortex. Dopamine is the neurotransmitter on the nerve endings of the nigrostriatal fibers. Parkinson disease is brought on by a reduction in the launch of dopamine throughout the corpus striatum. None of the efferent fibers from the corpus striatum descend on to the motor nuclei of the cranial nerves. The activities of the globus pallidus precede the activities of the motor cerebral cortex involved with discrete actions of the arms and feet. The outflow of the basal nuclei is channeled through the globus pallidus to the motor areas of the cerebral cortex, thus influencing muscular actions. The activities of the basal nuclei are initiated by data obtained from the sensory cortex, the thalamus, and the brainstem. The unique physician grouped collectively the facial paralysis, the slurred speech, and the hypertension and, within the absence of other findings, made the wrong analysis of cerebral hemorrhage. A lesion of the corticonuclear fibers on one facet of the mind will trigger paralysis only of the muscles of the decrease a half of the alternative side of the face. This affected person has full paralysis of the complete proper facet of the face, which could solely be attributable to a lesion of the lower motor neuron. The appropriate diagnosis was Bell palsy, an irritation of the connective tissue sheath of the facial nerve, which briefly interfered with the capabilities of the axons of the proper facial nerve. This case offers a good instance of how knowledge of the central connec- tions of a cranial nerve enables a physician to make the correct analysis. The cranial nerves are commonly damaged by trauma or disease, and testing for their integrity types part of every physical examination. The oculomotor, trochlear, abducens, accessory, and hypoglossal nerves are completely motor. The trigeminal, facial, glossopharyngeal, and vagus nerves are each sensory and motor nerves. The letter symbols commonly used to point out the functional elements of each cranial nerve are shown in Table 11-1. The cranial nerves have central motor and/or sensory nuclei inside the mind and peripheral nerve fibers that emerge from the mind and exit from the cranium to reach their effector or sensory organs. The completely different elements of the cranial nerves, their features, and the openings in the cranium by way of which the nerves depart the cranial cavity are summarized in Table 11-2. Cranial Nerve Motor Nuclei the motor nuclei of the cranial nerves obtain impulses from the cerebral cortex via the corticonuclear 323 mebooksfree. These fibers originate from the pyramidal cells in the inferior a half of the precentral gyrus (area 4) and from the adjacent part of the postcen- tral gyrus. The corticonuclear fibers descend through the corona radiata and the genu of the interior capsule. They pass through the midbrain just medial to the corticospinal fibers within the foundation pedunculi and end by synapsing both directly with the decrease motor neurons inside the cranial nerve nuclei or not directly through the internuncial neurons. The corticonuclear fibers thus constitute the first-order neuron of the descending pathway, the internuncial neuron constitutes the secondorder neuron, and the lower motor neuron constitutes the mind. Such a nerve cell is, subsequently, equal to the motor cells within the anterior gray columns of the spinal twine. The majority of the corticonuclear fibers to the motor cranial nerve nuclei cross the median airplane before reaching the nuclei. Bilateral connections are current for all of the cranial motor nuclei except for part of the facial nucleus that supplies the muscle tissue of the lower part of the face and part of the hypoglossal nucleus that supplies the genioglossus muscle. The common visceral motor nuclei kind the cranial outflow of the parasympathetic portion of the autonomic nervous system. They are the Edinger-Westphal nucleus of the oculomotor nerve, the superior salivatory and lacrimal nuclei of the facial nerve, the inferior salivatory nucleus of the glossopharyngeal nerve, and the dorsal motor nucleus of the vagus. These nuclei receive numerous afferent fibers, including descending pathways from the hypothalamus. The somatic motor and branchiomotor nerve fibers of a cranial nerve are the axons of nerve cells located inside Sensory nuclei of the cranial nerves embody somatic and visceral afferent nuclei. The sensory or afferent elements of a cranial nerve are the axons of nerve cells exterior the brain and are located in ganglia on the nerve trunks (equivalent to posterior root ganglion of a spinal nerve) or could also be situated in a sensory organ, such because the nose, eye, or ear. The central processes of these cells enter the brain and terminate by synapsing with cells forming the sensory nuclei. Each receptor cell consists of a small bipolar nerve cell with Granular cell Synaptic glomerulus Tufted cell the place they synapse. The nerve cells of those nuclei type the third-order neuron, and their axons terminate in the cerebral cortex. From the coarse peripheral process, a quantity of quick cilia arise, the olfactory hairs, which project into the mucus overlaying the surface of the mucous membrane. These projecting hairs react to odors in the air and stimulate the olfactory cells. Bundles of these nerve fibers move via the openings of the cribriform plate of the ethmoid bone to enter the olfactory bulb. The fibers of the optic nerve are myelinated, but the sheaths are shaped from oligodendrocytes somewhat than Schwann cells, since the optic nerve is corresponding to a tract within the central nervous system. The optic nerve leaves the orbital cavity by way of the optic canal and unites with the optic nerve of the other side to kind the optic chiasma. Optic Chiasma the optic chiasma is located at the junction of the anterior wall and flooring of the third ventricle. In the chiasma, the fibers from the nasal (medial) half of every retina, together with the nasal half of the macula, cross the midline and enter the optic tract of the alternative facet, whereas the fibers from the temporal (lateral) half of each retina, together with the temporal half of the macula, cross posteriorly in the optic tract of the same aspect. Olfactory Bulb this ovoid construction possesses a number of forms of nerve cells, the largest of which is the mitral cell. The incoming olfactory nerve fibers synapse with the dendrites of the mitral cells and type rounded areas generally known as synaptic glomeruli. Smaller nerve cells, referred to as tufted cells and granular cells, also synapse with the mitral cells. The olfactory bulb, as well as, receives axons from the contralateral olfactory bulb via the olfactory tract. Olfactory Tract this slim band of white matter runs from the posterior finish of the olfactory bulb beneath the inferior floor of the frontal lobe of the brain. It consists of the axons of the mitral and tufted cells of the bulb and a few centrifugal fibers from the other olfactory bulb. As the olfactory tract reaches the anterior perforated substance, it divides into medial and lateral Optic Tract the optic tract emerges from the optic chiasma and passes posterolaterally across the cerebral peduncle. Most of the fibers now terminate by synapsing with nerve cells in the lateral geniculate physique, which is a small projection from the posterior part of the thalamus. A few of the fibers cross to the pretectal nucleus and the superior colliculus of the midbrain and are concerned with gentle reflexes. The lateral stria carries the axons to the olfactory space of the cerebral cortex, particularly, the Lateral Geniculate Body the lateral geniculate physique is a small, oval swelling projecting from the pulvinar of the thalamus. It consists of six layers of cells, on which synapse the axons from the optic tract. The axons of the nerve cells throughout the geniculate body depart it to type the optic radiation.
Birangasifa (Yarrow). Stromectol.
- Are there safety concerns?
- Are there any interactions with medications?
- How does Yarrow work?
- Fever, common cold, hayfever, diarrhea, stomach discomfort, bloating, gas, toothache, and other conditions.
- What is Yarrow?
- Dosing considerations for Yarrow.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96188
The connections and useful significance of those nuclei are described in Chapter eleven viral infection 07999 stromectol 6 mg with visa. They receive nerve fibers from the cerebral cortex and send efferent fibers to the cerebellum by way of the anterior external arcuate fibers antibiotics for recurrent uti stromectol 3 mg buy generic line. The pyramids containing the corticospinal and a few corticonuclear fibers are located within the anterior a part of the medulla separated by the anterior median fissure antibiotic home remedies buy discount stromectol 12 mg. The medial lemniscus varieties a flattened tract on each side of the midline posterior to the pyramid infection 4 weeks after miscarriage generic 12 mg stromectol fast delivery. These fibers emerge from the decussation of the lemnisci and convey sensory information to the thalamus. The medial longitudinal fasciculus varieties a small tract of nerve fibers located on both sides of the midline posterior to the medial lemniscus and anterior to the hypoglossal nucleus. It consists of ascending and descending fibers, the connections of that are described on page 205. The inferior cerebellar peduncle is situated in the posterolateral nook of the section on the lateral aspect of the fourth ventricle. The spinal tract of the trigeminal nerve and its nucleus are situated on the anteromedial side of the inferior cerebellar peduncle. The anterior spinocerebellar tract is located near the floor within the interval between the inferior olivary nucleus and the nucleus of the spinal tract of the trigeminal nerve. The spinal lemniscus, consisting of the anterior spinothalamic, the lateral spinothalamic, and spinotectal tracts, is deeply placed. The reticular formation, consisting of a diffuse mixture of nerve fibers and small teams of nerve cells, is deeply placed posterior to the olivary nucleus. The reticular formation represents, at this stage, solely a small part of this technique, which is also present within the pons and midbrain. The glossopharyngeal, vagus, and cranial a part of the accent nerves may be seen running ahead and laterally via the reticular formation. The hypoglossal nerves additionally run anteriorly and laterally by way of the reticular formation and emerge between the pyramids and the olives. The lateral vestibular nucleus has replaced the inferior vestibular nucleus, and the cochlear nuclei now are seen on the anterior and posterior surfaces of the inferior cerebellar peduncle. The anterior surface is convex from side to side and shows many transverse fibers that converge on both sides to form the center cerebellar peduncle. On the anterolateral surface of the pons, the trigeminal nerve emerges on all sides. Each nerve consists of a smaller, medial part, generally recognized as the motor root, and a bigger, lateral part, known as the sensory root. In the groove between the pons and the medulla In comparability to the previous stage, little modifications within the distribution of the gray and white matter. Hypoglossal nerve Medulla oblongata Anterior surface of the brainstem displaying the pons. It forms the upper half of the floor of the fourth ventricle and is triangular in form. The posterior surface is limited laterally by the superior cerebellar peduncles and is split into symmetrical halves by a median sulcus. Lateral to this sulcus is an elongated elevation, the medial eminence, section via the cranial part, passing via the trigeminal nuclei. Table 5-3 compares the two levels of the pons and the most important structures current at each stage. The inferior end of the medial eminence is barely expanded to type the facial colliculus, which is produced by the root of the facial nerve winding around the nucleus of the abducens nerve. The ground of the superior part of the sulcus limitans is bluish-gray in colour and is identified as the substantia ferruginea; it owes its color to a bunch of deeply pigmented nerve cells. Lateral to the sulcus limitans is the world vestibuli produced by the underlying vestibular nuclei. Internal Structure For purposes of description, the pons is often divided into a posterior half, the tegmentum, and an anterior basal part by the transversely working fibers of the trapezoid body. The structure of the pons may be studied at two levels: (1) transverse part through the caudal part, passing by way of the facial colliculus, and (2) transverse the medial lemniscus rotates as it passes from the medulla into the pons. It is situated in the most anterior a half of the tegmentum, with its lengthy axis running transversely. The fibers of the facial nerve wind around the nucleus of the abducens nerve, producing the facial colliculus. The fibers of the facial nerve then pass anteriorly between the facial nucleus and the superior end of the nucleus of the spinal tract of the trigeminal nerve. The medial longitudinal fasciculus is located beneath the ground of the fourth ventricle on both facet of the midline. The medial longitudinal fasciculus is the principle pathway that connects the vestibular and cochlear nuclei with the nuclei controlling the extraocular muscles (oculomotor, trochlear, and abducens nuclei). The medial vestibular nucleus is situated lateral to the abducens nucleus and is in shut relationship to the inferior cerebellar peduncle. Transverse section by way of the caudal part of the pons at the level of the facial mebooksfree. The spinal nucleus of the trigeminal nerve and its tract lie on the anteromedial aspect of the inferior cerebellar peduncle. The trapezoid body is made up of fibers derived from the cochlear nuclei and the nuclei of the trapezoid body. The basilar a half of the pons, at this stage, accommodates and corticonuclear tracts, breaking them up into small bundles. The transverse fibers of the pons enter the middle cerebellar peduncle and are distributed to the cerebellar hemisphere. This connection types the main pathway linking the cerebral cortex to the cerebellum. The corticopontine fibers of the crus cerebri of the midbrain terminate in the pontine nuclei. The axons of these cells give origin to the transverse fibers of the pons, which cross the midline and intersect the corticospinal Medial longitudinal fasciculus the interior construction of the cranial a part of the pons is much like that seen at the caudal stage. The motor nucleus of the trigeminal nerve is located beneath the lateral part of the fourth ventricle throughout the reticular formation. The superior cerebellar peduncle is situated posterolateral to the motor nucleus of the trigeminal nerve. The getting into sensory fibers journey Decussation of trochlear nerve Medial longitudinal fasciculus. The lateral and spinal lemnisci lie on the lateral extremity of the medial lemniscus. These are rounded eminences which would possibly be divided into superior and inferior pairs by a vertical and a transverse groove. Its lengthy axis inclines anteriorly because it ascends via the opening in the tentorium cerebelli. The midbrain is traversed by a slender channel, the cerebral aqueduct, which is filled with cerebrospinal fluid. These are small-diameter nerves that wind around the lateral aspect of the midbrain to enter the lateral wall of the cavernous sinus. On the lateral facet of the midbrain, the superior and inferior brachia ascend in an anterolateral course. The superior brachium passes from the superior colliculus to the lateral geniculate body and the optic tract. The inferior brachium connects the inferior colliculus to the medial geniculate body. Note that the cerebral peduncles are subdivided by the substantia nigra into the tegmentum and the crus cerebri. On the anterior aspect of the midbrain, a deep melancholy within the midline, the interpeduncular fossa, is bounded on both facet by the crus cerebri. Many small blood vessels perforate the floor of the interpeduncular fossa, and this area is termed the posterior perforated substance. The oculomotor nerve emerges from a groove on the medial side of the crus cerebri and passes forward in the lateral wall of the cavernous sinus.