
Sustiva
| Contato
Página Inicial

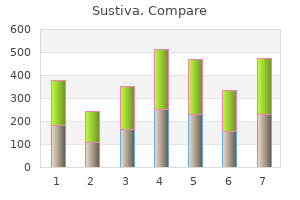
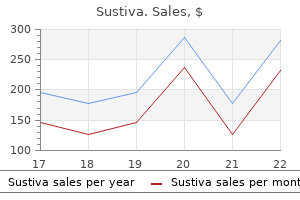
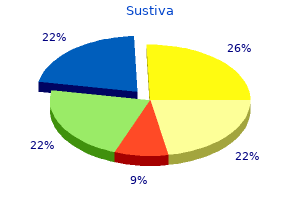
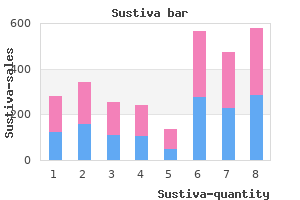
"Sustiva 600mg buy visa, symptoms xxy".
A. Ines, M.A.S., M.D.
Co-Director, University of Utah School of Medicine
Intraoperative Considerations the objective of intraoperative administration is to protect current hepatic function treatment integrity purchase sustiva 600mg overnight delivery. Some sufferers with viral hepatitis might exhibit increased central nervous system sensitivity to anesthetics medications requiring prior authorization proven 200mg sustiva, whereas alcoholic patients will often show cross-tolerance to each intravenous and volatile anesthetics medicine for diarrhea order sustiva 200 mg without a prescription. Alcoholic patients additionally require close cardiovascular monitoring because the cardiac depressant effects of alcohol are additive to those of anesthetics; furthermore symptoms during pregnancy 200 mg sustiva generic visa, alcoholic cardiomyopathy may be present in alcoholic sufferers. Inhalation anesthetics are usually preferable to intravenous brokers as a outcome of a lot of the latter are dependent on the liver for metabolism, elimination, or both. Standard induction doses of intravenous induction agents can generally be used as a end result of their motion is terminated by redistribution somewhat than metabolism or excretion. A prolonged period of motion, nonetheless, may be encountered with large or repeated doses of intravenous agents, particularly 2 opioids. Isoflurane and sevoflurane are the unstable agents of choice for patient with important liver illness as a end result of they preserve hepatic blood move and oxygen supply. Factors identified to cut back hepatic blood circulate, corresponding to hypotension, extreme sympathetic activation, and high mean airway pressures throughout controlled air flow, should be prevented. Regional anesthesia, including main conduction blockade, may be employed within the absence of coagulopathy, offered hypotension is avoided. Patients with chronic energetic hepatitis have chronic hepatic inflammation with destruction of regular mobile architecture "piecemeal necrosis" on the biopsy. Evidence of cirrhosis is both current initially or ultimately develops in 20% to 50% of sufferers. Although continual lively hepatitis seems to have many causes, it occurs most commonly as a sequela of hepatitis B or hepatitis C. Other causes embody medications (methyldopa, isoniazid, and nitrofurantoin) and autoimmune problems. Both immunological components and a genetic predisposition could also be accountable in most cases. Manifestations of cirrhosis ultimately predominate in patients with progressive illness. In 3 evaluating sufferers for chronic hepatitis, laboratory check outcomes could show only a light elevation in serum aminotransferase exercise and sometimes correlate poorly with disease severity. Patients without continual hepatitis B or C infection normally have a favorable response to immunosuppressants and are handled with long-term corticosteroid therapy with or with out azathioprine. Anesthetic Management Patients with chronic persistent or persistent lobular hepatitis ought to be handled equally to those with acute hepatitis. In contrast, these with persistent lively hepatitis ought to be assumed to already have cirrhosis and should be handled accordingly (as mentioned next). Patients can usually be categorized as having considered one of three distinct syndromes primarily based on a liver biopsy: persistent persistent hepatitis, chronic lobular Cirrhosis the liver of inflammation, hepatocellular injury, and the resulting fibrosis and regeneration of hepatocytes. Other causes embrace persistent active hepatitis (postnecrotic cirrhosis), persistent biliary inflammation or obstruction (primary biliary cirrhosis, sclerosing cholangitis), continual right-sided congestive heart failure (cardiac cirrhosis), autoimmune hepatitis, hemochromatosis, Wilson illness, 1-antitrypsin deficiency, and cryptogenic cirrhosis. Regardless of the trigger, hepatocyte necrosis is adopted by fibrosis 5 and nodular regeneration. Manifestations are usually absent initially, however jaundice and ascites ultimately develop in most sufferers. Other indicators include spider angiomas, palmar erythema, gynecomastia, and splenomegaly. Moreover, cirrhosis is usually related to the event of three main issues: (1) variceal hemorrhage from portal hypertension, (2) intractable fluid retention in the form of ascites and the hepatorenal syndrome, and (3) hepatic encephalopathy or coma. Approximately 10% of patients with cirrhosis also develop at least one episode of spontaneous bacterial peritonitis, and a few sufferers eventually develop hepatocellular carcinoma. A few ailments can produce hepatic fibrosis without hepatocellular necrosis or nodular regeneration, resulting in portal hypertension and its related issues with hepatocellular function often preserved. These problems embrace schistosomiasis, idiopathic portal fibrosis (Banti syndrome), and congenital hepatic fibrosis. Obstruction of the hepatic veins or inferior vena cava (Budd�Chiari syndrome) can even trigger portal hypertension. The latter may be the outcome of venous thrombosis (hypercoagulable state), a tumor thrombus (eg, renal carcinoma), or occlusive disease of the sublobular hepatic veins. Preoperative Considerations the detrimental effects of anesthesia and surgery on hepatic blood move are discussed later in this section. Patients with cirrhosis are at elevated risk of degradation of liver perform due to limited functional reserve. Successful anesthetic management of these patients depends on recognizing the multisystem nature of cirrhosis (Table 34�3) and controlling or stopping its complications. Gastrointestinal Manifestations Portal hypertension leads to the development of intensive portosystemic venous collateral channels. Four major collateral sites are generally recognized: gastroesophageal, hemorrhoidal, periumbilical, and retroperitoneal. Portal hypertension is usually obvious preoperatively, as evidenced by dilated abdomi6 nal wall veins (caput medusae). Massive bleeding from gastroesophageal varices is a significant cause of morbidity and mortality in sufferers with liver illness, and, in addition to the consequences of acute blood loss, the absorbed nitrogen load from the breakdown of blood within the gastrointestinal tract can precipitate hepatic encephalopathy. The therapy of variceal bleeding is primarily supportive, but incessantly includes endoscopic procedures for identification of the bleeding site(s) and therapeutic maneuvers, such as injection sclerosis of varices, monopolar and bipolar electrocoagulation, or application of hemoclips or bands. Endoscopic unipolar electrocautery could adversely affect implanted cardiac pacing and defibrillator units. Nonoperative therapy consists of vasopressin, somatostatin, propranolol, and balloon tamponade with a Sengstaken�Blakemore tube. High doses of vasopressin can lead to congestive heart failure or myocardial ischemia; concomitant infusion of intravenous nitroglycerin might reduce the chance of these problems and bleeding. Perioperative risk correlates with diploma of hepatic impairment, based mostly on clinical and laboratory findings. Shunting procedures are typically carried out on low-risk patients, whereas ablative surgery, esophageal transection, and gastric devascularization are reserved for high-risk sufferers. Hematologic Manifestations Anemia, thrombocytopenia, and, less generally, leukopenia could also be present. The reason for the anemia is often multifactorial and contains blood loss, increased pink blood cell destruction, bone marrow suppression, and nutritional deficiencies. Congestive splenomegaly secondary to portal hypertension is largely responsible for the thrombocytopenia and leukopenia. Enhanced fibrinolysis secondary to decreased clearance of activators of the fibrinolytic system may contribute to the coagulopathy. Protein breakdown from excessive blood transfusions can precipitate encephalopathy. Clotting elements must be changed with acceptable blood merchandise, corresponding to contemporary frozen plasma and cryoprecipitate. Platelet transfusions must be considered instantly previous to surgical procedure for platelet counts lower than seventy five,000/L. Assessment of integrity of the coagulation system by viscoelastic know-how will present specific management info. Increased cardiac output Increased coronary heart fee Decreased systemic vascular resistance Increased circulating volume Coronary artery disease Cirrhotic cardiomyopathy (often unrecognized) Low systemic vascular resistance conceals poor left ventricular function Reduced responsiveness to -agonists C. Circulatory Manifestations End-stage liver illness, and in particular, cirrhosis of the liver could also be related to issues of all main organ systems (Tables 34�3 and 34�5). Cardiovascular changes noticed in cirrhotic sufferers 7 are often those of a hyperdynamic circulation, though clinically significant cirrhotic cardiomyopathy is usually present and not acknowledged (Table 34�6). There could also be a reduced cardiac contractile response to stress, altered diastolic leisure, downregulation of -adrenergic receptors, and electrophysiological adjustments on account of cirrhotic cardiomyopathy. Echocardiographic examination of cardiac function may initially be interpreted as regular due to significant afterload discount brought on by low systemic vascular resistance. Noninvasive stress imaging is incessantly used to assess coronary artery disease in patients older than age 50 years and in these with cardiac risk components. Intrapulmonary vascular dilation causes intrapulmonary right-to-left shunting and a rise in the alveolar-to-arterial oxygen gradient. Increased pulmonary vascular resistance: vasoconstriction, structural vascular remodeling, and eventual fibrosis Mean pulmonary artery stress >25 mm Hg with regular pulmonary capillary wedge strain Right ventricular overload Right coronary heart failure Hepatic congestion Increased liver transplantation mortality danger, particularly if mean pulmonary artery strain is >35 mm Hg easy muscle proliferation, vasoconstriction, intimal proliferation, and eventual fibrosis, all presenting as obstruction causing an elevated resistance to pulmonary blood flow. In some patients, pulmonary hypertension will reverse shortly after transplant; however, other patients may require months or years of ongoing vasodilator therapy. Respiratory Manifestations Disturbances in pulmonary gasoline exchange and ventilatory mechanics are sometimes present. As previously noted, hypoxemia is incessantly present and is due to right-to-left shunting of as much as 40% of cardiac output.
Epidural steroid injections may be handiest when the injection is on the website of harm treatment notes order sustiva 200mg free shipping. Larger or more frequent doses increase the chance of adrenal suppression and systemic unwanted effects symptoms ruptured spleen discount sustiva 600mg without prescription. A transforaminal epidural steroid injection may be simpler than the standard interlaminar epidural method medications ok during pregnancy generic sustiva 200 mg overnight delivery, particularly for radicular pain medicine zocor sustiva 200mg buy cheap on line. The needle is directed underneath fluoroscopic steerage into the foramen of the affected nerve root; contrast is then injected to affirm unfold into the epidural area and absence of intravascular injection prior to steroid injection. Note the Tuohy needle superior simply to the best of midline for remedy of degenerative disc disease and proper radicular pain. Live fluoroscopy is used to reduce the chance of inadvertent intravascular injection. The epidural injection of distinction adopted by native anesthetic and steroid solution leads to unfold at multiple ranges of the epidural house and through the neuroforamen. Unfortunately, migration of the steroid to the location of injury may not be optimum because of anatomic distortion of the epidural area. The use of a catheter to extra exactly direct the injection inside the sacral and epidural canal could improve end result. Electrical stimulation (2 Hz for motor responses, 50 Hz for sensory responses) and impedance measurement by way of the electrode previous to ablation also help confirm correct electrode positioning. Depending on the placement of the block, the heating temperature generated at the electrode is precisely managed (60�90�C for 1�3 min) to ablate the nerve without causing extreme collateral tissue damage. It has also been used for dorsal root rhizotomy and lumbar sympathectomy, and could also be effective for medial branches of the spinal nerves that innervate facet joints. Pulsed radiofrequency at 42�C can be being evaluated for numerous ache conditions. Cryoneurolysis may produce temporary analgesia (cryoanalgesia) for weeks to months by freezing and thawing tissue. The temperature on the tip of a cryoprobe rapidly drops as carbon dioxide or nitrous oxide gas at high stress is allowed to expand. The probe tip, which can obtain temperatures of �50�C to �70�C, is introduced via a 12- to 16-gauge catheter. Electrical stimulation (2�5 Hz for motor responses and 50�100 Hz for sensory responses) helps affirm right positioning of the probe. Cryoneurolysis is mostly used to achieve long-term blockade of peripheral nerves and could additionally be significantly helpful for post-thoracotomy pain. Diagnostic intercostal nerve blocks may be useful to determine the nerve(s) that may be contributing to persistent thoracic or abdominal pain, and intercostal nerve blocks can also be utilized for longer term analgesia. The principal dangers of intercostal nerve blocks are pneumothorax and native anesthetic toxicity. Chemical Neurolysis with extreme, intractable most cancers ache in whom extra standard therapy proves insufficient or standard analgesic modalities are accompanied by unacceptable unwanted effects. The most typical chemical neurolytic techniques utilized for most cancers sufferers are celiac plexus, lumbar sympathetic chain, hypogastric plexus, and ganglion impar blocks. Chemical neurolysis can also often be used in sufferers with refractory benign neuralgia and, rarely, in patients with peripheral vascular disease. These blocks can be related to considerable morbidity (loss of motor and sensory function), so patients should be chosen fastidiously, and solely after thorough consideration of alternative analgesic modalities. Moreover, although the preliminary end result may be glorious, the unique pain may recur or new (deafferentation or central) ache develop in a majority of sufferers within weeks to months. Temporary destruction of nerve fibers or ganglia could be accomplished by injection of alcohol or phenol. Ethyl alcohol 50% to 100 percent causes extraction of membrane phospholipids and precipitation of lipoproteins in axons and Schwann cells, whereas phenol 6% to 12% coagulates proteins. Alcohol causes extreme ache on injection; thus native anesthetic is normally administered first. Phenol is often painless when injected both as a 6% or an 8% aqueous answer or in glycerol; a 12% phenol solution could be prepared in radiopaque distinction answer. Neurolytic intercostal blocks may be useful for sufferers with painful rib metastases. Additional neurodestructive procedures, similar to pituitary adenolysis and cordotomy, could additionally be useful in end-of-life palliative care. When contemplating any neurolytic approach, a minimum of one diagnostic block with an area anesthetic resolution alone must be used initially to affirm the pain pathway(s) concerned and to assess the potential efficacy and morbidity of the deliberate neurolysis. Local anesthetic solution should once more be injected instantly previous to the neurolytic agent underneath fluoroscopic steerage. Following injection of any neurolytic agent, the needle must be cleared with air or saline previous to withdrawal to stop damage to superficial structures. Many clinicians favor alcohol for celiac plexus block and phenol for lumbar sympathetic block. For subarachnoid neurolytic techniques, very small quantities of neurolytic agent (0. Alcohol is hypobaric, whereas phenol in glycerin is hyperbaric; the patient undergoing subarachnoid neurolysis is rigorously positioned in order that the answer travels to the suitable degree and is confined to the dorsal horn region following subarachnoid administration. When such a patient has discontinued anticoagulant treatment in preparation for a diagnostic local anesthetic block, it might be extra sensible to acquire consent for a neurolytic process prematurely and to observe the diagnostic block instantly with chemical neurolysis if the diagnostic procedure has resulted in ache relief. Neurolytic Techniques Neurolytic celiac plexus or splanchnic nerve blocks may be effective for painful intraabdominal neoplasms, particularly pancreatic cancer. Lumbar sympathetic, hypogastric plexus, or ganglion impar neurolytic blocks can be used for pain secondary to pelvic neoplasms. Neurolytic saddle block can provide pain relief for patients with refractory pain from pelvic malignancy; nevertheless, bowel and 7. Differential Neural Blockade Pharmacological or anatomic differential neural blockade has been advocated as a method of distinguishing somatic, sympathetic, and psychogenic pain mechanisms. The procedure is controversial owing to the challenges of deciphering the information and the lack to define precisely which nerve fibers or pathways are blocked. Theoretically, the pharmacological approach relies on the differential sensitivity of nerve fibers to local anesthetics. By utilizing completely different concentrations of native anesthetic, it might be potential to selectively block sure forms of fibers while preserving the function of others. The challenge is that the crucial focus needed to block sympathetic fibers can differ significantly between patients, and conduction block by native anesthetics is dependent not only on fiber measurement but in addition on the period of contact and frequency of impulses carried out. Many clinicians have due to this fact deserted the usage of pharmacological differential neural blocks in favor of anatomic differential blockade. Stellate ganglion blocks can be utilized to selectively block sympathetic fibers to the top, neck, and arm. Celiac plexus, hypogastric plexus, and lumbar paravertebral sympathetic blocks can be used for sympathetic blocks of the abdomen, pelvis, and leg, respectively. Selective nerve root, intercostal, cervical plexus, brachial plexus, or lumbosacral plexus blocks may be used for somatic nerve blockade. Differential epidural blocks may be used for thoracic pain when the strategies for sympathetic blockade carry a significant threat of pneumothorax (Table 47�16). After every epidural injection, the patient is evaluated for ache reduction, signs of sympathetic blockade (a decrease in blood pressure), sensation to pinprick and light contact, and motor operate. If the ache disappears after the saline injection, the affected person both has psychogenic ache (usually a profound long-lasting effect) or is displaying a placebo effect (usually short lasting). Lastly, if the ache persists even after indicators of motor blockade, the ache is both central (supraspinal) or psychogenic. The differential epidural block carries the risk of any neuraxial block, and the possibility of hypotension and blocking cardiac accelerator fibers at T1�T4. Following catheter insertion, injections should be administered with the affected person in a monitored setting for the rest of this procedure. Although differential epidural blockade has limitations, it may be helpful to identify primarily centralized ache when a patient continues to have a significant degree of ache regardless of multilevel dermatomal blockade over the painful area. It is unlikely that a subsequent nerve block would assist to treat the painful situation. This could provide potential short- or longterm aid and may be thought of as a substitute for differential epidural blockade. Neuromodulation Electrical stimulation of the nervous system can produce analgesia in sufferers with acute and persistent ache. Current may be applied transcutaneously, epidurally, or by electrodes implanted into the central nervous system.
Lidocaine infusions are used in some facilities as a supplement to basic anesthesia to reduce emergence delirium and the requirement for opioids medicine 8162 generic sustiva 600 mg with amex. This improves preservation of metabolism and upkeep of the mitochondrial transmembrane potential (3) treatment meaning sustiva 200mg buy low cost. A higher preservation of synaptic proteins happens symptoms 8-10 dpo buy sustiva 600mg free shipping, and the expression of progress proteins indicating regeneration in grownup neurons is enhanced (6 medications made from animals sustiva 600mg buy with amex, 7). Reversal of narcotics or benzodiazepines in continual customers can lead to symptoms of substance withdrawal. Excessive elevations in blood stress with any agent can disrupt the blood�brain barrier. Interruption of cerebral perfusion, metabolic substrate (glucose), or severe hypoxemia rapidly ends in functional impairment; reduced perfusion additionally impairs clearance of doubtless toxic metabolites. Sustained will increase in intracellular Ca2+ activate lipases and proteases, which provoke and propagate structural harm to neurons. Increases in free fatty acid concentration and cyclooxygenase and lipoxygenase actions end result in the formation of prostaglandins and leukotrienes, a few of which are potent 9 With normal autoregulation and an intact 10 the brain could be very susceptible to ischemic harm four. Accumulation of poisonous metabolites impairs cellular function and interferes with repair mechanisms. Lastly, reperfusion of ischemic tissues may cause additional tissue damage because of the formation of oxygen-derived free radicals. Likewise, inflammation and edema can promote further neuronal injury, leading to cellular apoptosis. Global ischemia could result from total circulatory arrest as properly as global hypoxia. Cessation of perfusion may be attributable to cardiac arrest or deliberate circulatory arrest, whereas world hypoxia may be attributable to severe respiratory failure, drowning, and asphyxia (including anesthetic mishaps). Focal ischemia contains embolic, hemorrhagic, and atherosclerotic strokes, as nicely as blunt, penetrating, and surgical trauma. In some cases, interventions aimed toward restoring perfusion and oxygenation are potential; these embody reestablishing efficient circulation, normalizing arterial oxygenation and oxygencarrying capacity, or reopening and stenting an occluded vessel. With focal ischemia, the brain tissue surrounding a severely broken space may undergo marked useful impairment but still remain viable. Such areas are thought to have very marginal perfusion (<15 mL/100 g/min), however, if additional harm could be limited and normal move is rapidly restored, these areas (the "ischemic penumbra") may recover completely. From a sensible perspective, efforts geared toward stopping or limiting neuronal tissue harm are often related whether the ischemia is focal or global. Clearly, the best technique is prevention, as a end result of once harm has occurred, measures aimed at cerebral safety turn out to be less effective. Indeed, profound hypothermia is often used for up to 1 h of complete circulatory arrest. Unlike anesthetic brokers, hypothermia decreases both basal and electrical metabolic necessities throughout the brain; metabolic requirements proceed to decrease even after full electrical silence. Additionally, hypothermia reduces free radicals and other mediators of ischemic damage. Induced hypothermia has shown benefit following cardiac arrest and is a routine part of most post-arrest protocols for comatose patients. Anesthetic Agents Barbiturates, etomidate, propofol, isoflurane, desflurane, and sevoflurane can produce burst suppression, and all however desflurane and sevoflurane can produce full electrical silence of the brain and eliminate the metabolic cost of electrical exercise. Furthermore, aside from barbiturates, their results are nonuniform, affecting totally different components of the mind to variable extents. No anesthetic agent has consistently been shown to be protective in opposition to international ischemia. Studies highlighting the potential neurotoxicity of anesthetics (especially in infants) additionally query the function of risky anesthetics in neuroprotection. Specific Adjuncts Nimodipine plays a task within the within the remedy of vasospasm associated with subarachnoid hemorrhage. General Measures General patient management strategies are the neuroanesthesia interventions most likely to improve affected person outcomes. Hyperglycemia aggravates neurological injuries following either focal or international ischemia, and blood glucose ought to be maintained at lower than a hundred and eighty mg/dL. The most commonly used monitor throughout neurosurgical procedures is evoked potentials. Proper software of those monitoring modalities is critically dependent on recognizing anestheticinduced modifications. Inhalation Anesthetics Isoflurane, desflurane, and sevoflurane produce a burst suppression sample at excessive doses (>1. Nitrous oxide is uncommon in that it increases both frequency and amplitude (high-amplitude activation). Barbiturates, etomidate, and propofol produce a similar pattern and are the one commonly used intravenous brokers capable of producing burst suppression and electrical silence at excessive doses. Lastly, ketamine produces an uncommon activation consisting of rhythmic high-amplitude theta activity adopted by very high-amplitude gamma and low-amplitude beta actions. The adequacy of perfusion of the spinal cord throughout aortic surgery is better assessed with motor evoked potentials (which assess the anterior part of the spinal cord). Visual evoked potentials may be used to monitor the optic nerve and occipital cortex during resections of large pituitary tumors. Evoked potentials have poststimulus latencies which may be described as brief, intermediate, and lengthy. Intermediate- and long-latency evoked potentials are primarily of cortical origin. In common, short-latency potentials are least affected by anesthetic brokers, whereas long-latency potentials are affected by even subanesthetic ranges of most brokers. Visual evoked potentials are most affected by anesthetics, whereas brainstem auditory evoked potentials are least affected. Intravenous brokers in scientific doses typically have much less marked results on evoked potentials than do unstable brokers, however, in excessive doses, can also decrease amplitude and improve latencies (see Chapter 6). This affected person might properly have been weak on the left aspect prior to surgery, in which case the hemiparesis may be as a outcome of a preexisting condition. General anesthesia was chosen because many surgeons working within the neck area felt more comfy if the airway was managed, and the patient was fully anesthetized ought to proof of cerebral ischemia develop. More just lately, regional anesthesia has been advocated as offering an adequate surgical area, a snug and relaxed patient (if done with monitored anesthesia care), secure hemodynamics, and perfect monitoring of cerebral perform during crossclamping as a result of an awake affected person supplies one of the best proof of enough cerebral perfusion. The affected person can indicate or be noticed for proof of aphasia, facial droop, or hemiparesis. Patients with carotid stenosis are at very elevated threat of coronary artery and peripheral arterial disease. In sufferers present process common anesthesia, indirect cerebral monitoring strategies have been used to assess the adequacy of the cerebral circulation. Back bleeding of the distal carotid artery following crossclamp and incision of the artery suggests reasonable collateral circulation above the clamp. Some surgeons consider that a shunt ought to be used in all patients with a previous cerebrovascular accident, unbiased of stump pressure, and for any affected person whose stump pressure is less than 25 mm Hg. However, that is controversial, as many neurosurgeons and vascular surgeons use 50 mm Hg as a cutoff. The reliability of stump pressure to predict the necessity for selective shunting has additionally been questioned. Some surgeons routinely shunt all sufferers, some shunt no patients, and others use selective shunting. Should neurophysiological studies identify cerebral ischemia, the surgeon can place a vascular shunt through the surgical restore to present for ipsilateral cerebral perfusion. During carotid clamping and instantly afterward in the restoration room, patients are sometimes hemodynamically labile. Bradycardia can develop during surgical manipulation of the carotid sinus due to the direct stimulation of the vagus nerve. Tachycardia could develop because of stress or ache or as a direct result of manipulation of the carotid sinus with release of catecholamines into the circulation. Hypotension can also be noticed because of the direct vasodilating and unfavorable ionotropic effects of anesthetic agents. Hypotension following carotid unclamping is frequent, particularly in patients with more severe carotid stenosis. Cerebral autoregulation protects the brain from reperfusion by decreasing manufacturing of renin, vasopressin, and norepinephrine, which leads to hypotension. Many sufferers have hypertension as a comorbid condition, which is often further exacerbated by the surgical stress and manipulation of the carotid physique, which causes release of catecholamines and sympathetic stimulation.
Anesthetic Technique the cirrhotic liver is very depending on hepatic arterial perfusion because of decreased portal venous C medicine 81 200mg sustiva buy overnight delivery. Monitoring Pulse oximetry should be supplemented with arterial blood fuel measurements to monitor acid�base standing medicine shoppe order sustiva 600mg online. Patients receiving vasopressin infusions ought to be monitored for myocardial ischemia as a outcome of symptoms low potassium discount sustiva 200 mg on-line coronary vasoconstriction medications known to cause weight gain sustiva 600 mg purchase with visa. Continuous intraarterial stress monitoring is commonly used as a end result of hemodynamic instability regularly happens on account of extreme bleeding and operative manipulations. Urinary output must be followed closely; mannitol could also be thought of for persistently low urinary outputs regardless of adequate intravascular fluid substitute. Fluid Replacement Most patients are sodium-restricted preoperatively, but preservation of intravascular volume and urinary output takes precedence intraoperatively. The use of predominantly colloid intravenous fluids (albumin) could additionally be preferable to avoid sodium overload and to enhance plasma oncotic strain. Intravenous fluid replacement ought to keep in mind the extreme bleeding and fluid shifts that usually happen in these patients throughout belly procedures. Venous engorgement from portal hypertension, varices, lysis of adhesions from previous surgery, and coagulopathy lead to excessive bleeding throughout surgical procedures, whereas evacuation of ascites and prolonged surgical procedures result in giant fluid shifts. Liberal use of crystalloid solutions might lead to widespread edema due to the low serum albumin, and colloid solutions are normally more applicable. Most preoperative sufferers are anemic and coagulopathic, and perioperative purple blood cell transfusion may lead to hypocalcemia from impaired citrate metabolism in the cirrhotic liver. Citrate, the anticoagulant in stored pink blood cell preparations, binds with plasma calcium, producing hypocalcemia. Hepatic Surgery Common hepatic procedures include restore of lacerations, drainage of abscesses, and resection of primary or metastatic neoplasms, and as much as 80% to 85% of the liver can be resected in many sufferers. The perioperative care of patients undergoing hepatic surgical procedure is usually challenging due to coexisting medical problems and debilitation discovered in plenty of sufferers with intrinsic liver disease, and because of the potential for significant operative blood loss. Hepatitis and cirrhosis significantly complicate anesthetic administration and enhance perioperative mortality. Multiple large-bore intravenous catheters and fluid blood heaters are needed; speedy infusion gadgets facilitate management when large blood transfusion is anticipated. Hemodynamic optimization is commonly difficult by the conflict between the necessity to maintain sufficient intravascular quantity to ensure adequate hepatic perfusion and the need to keep central venous strain low to reduce liver engorgement and surgical bleeding. Hypotensive anesthesia ought to be prevented because of its probably deleterious effects on liver function. Administration of antifibrinolytics, such as -aminocaproic acid or tranexamic acid, may cut back operative blood loss, especially if fibrinolysis could be demonstrated by viscoelastic coagulation monitoring. Hypoglycemia, coagulopathy, and sepsis might occur following massive liver resections. In the case of a hydatid cyst, spillage can cause anaphylaxis because of the release of Echinococcus antigens. Postoperative problems embody hepatic dysfunction, sepsis, and blood loss secondary to coagulopathy or surgical bleeding. Postoperative pain from the surgical incision could hinder postoperative mobilization and convalescence, but perioperative coagulopathy might restrict using epidural analgesia. Liver Transplantation When a middle opens a liver transplantation program, a credentialed director ought to be appointed who must be an anesthesiologist with experience and coaching in liver transplantation anesthesia. These sufferers usually have an elevated cardiac index and reduced systemic vascular resistance. Significant blood loss could additionally be anticipated, and large-bore intravenous catheters ought to be positioned for entry. It has been demonstrated that such an approach improves outcomes, as measured by reduced blood transfusions, the necessity for postoperative mechanical air flow, and the intensive care unit length of keep. Therefore, each organ should be fastidiously managed all through the operative procedure and postoperative period. Additional cerebral protective measures embrace head elevation of 20�, mild hypothermia, and mild hypocarbia with vasopressor assist to keep imply arterial strain. Blood loss may be massive, and transfusions are focused to preserve the hemoglobin level at higher than 7 g/dL. Fibrinolysis, a low ionized calcium stage, and hypothermia should be corrected, as these might promote bleeding. Intraoperative transfusion of platelets and contemporary frozen plasma is associated with decreased long-term patient survival. The liver transplantation surgical process is split into three levels: the dissection (preanhepatic), anhepatic, and neohepatic periods. The dissection (preanhepatic) phase is highlighted by the management of hemodynamic modifications associated to blood loss and surgical compression of main vessels. Hyponatremia should be carefully managed with out fast serum sodium correction, as a outcome of this will promote the event of osmotic demyelination syndrome. The anhepatic part begins with the vascular occlusion of the inflow to the liver and ends with reperfusion. Some centers utilize venovenous bypass to forestall congestion of the visceral organs, enhance venous return, and possibly defend kidney function. In the neohepatic part, two pathophysiological occasions might happen on opening the portal vein and permitting reperfusion of the graft. The first is a reperfusion syndrome brought on by the cold, acidotic, hyperkalemic solution that will comprise emboli and vasoactive substances being flushed from the graft directly into the vena cava. This might trigger hypotension, proper heart dysfunction, arrhythmias, and even cardiac arrest, and may be preempted to some extent by the prophylactic administration of calcium chloride and sodium bicarbonate. This could outcome from impaired reperfusion because of extreme endothelial dysfunction, and, in rare cases, might result in major nonfunction of the graft. The use of reduced-size and residing donor grafts has increased the organ availability in this affected person population. Postoperative Management Patients who endure liver transplantation are often severely debilitated and malnourished and have multiorgan dysfunction. A close watch of graft function have to be maintained, with a low threshold for checking hepatic artery patency and flow. Postoperative bleeding, biliary leaks, and vascular thromboses might require surgical reexploration. Living Donor Transplantation the use of living donors has increased the pool of organs obtainable for transplantation. However, this procedure does expose healthy people to morbidity and mortality risks. Adequate postoperative analgesia is required in order that comfortable donor patients may be extubated at the finish of the procedure. Complications of this surgery for the donor affected person embody transient hepatic dysfunction, wound infection, postoperative bleeding, portal vein thrombosis, biliary leaks, and, rarely, dying. An increased incidence of perioperative brachial plexus injury has been reported in donor patients. Orthotopic liver transplantation is usually carried out in patients with end-stage liver disease who start to expertise life-threatening problems, especially when such complications turn out to be unresponsive to medical or nontransplant surgical procedure. Transplantation can be carried out in sufferers with fulminant hepatic failure (from viral hepatitis or a hepatotoxin) when survival with medical management alone is judged unlikely. The commonest indications for liver transplantation in kids, so as of lowering frequency, are biliary atresia, inborn errors of metabolism (usually 1-antitrypsin deficiency, Wilson illness, tyrosinemia, and Crigler�Najjar type I syndrome), and postnecrotic cirrhosis. The most typical indications in adults are postnecrotic (nonalcoholic) cirrhosis, major biliary cirrhosis, and sclerosing cholangitis, and, less commonly, primary malignant tumors within the liver. One-year survival rates for liver transplantations exceed 80% to 85% in some facilities. The success of this process owes much to the usage of cyclosporine and tacrolimus for immunosuppressant remedy. Cyclosporine is often initially combined with corticosteroids and other brokers (eg, mycophenolate and azathioprine). Tacrolimus has proved efficient in cyclosporine-resistant rejection and is the preferred different to cyclosporine as the primary immunosuppressant agent. Additional elements influencing the advance in liver transplantation outcome embrace a higher understanding and experience with transplantation and improved assessment and monitoring with echocardiography. These procedures could be divided into three phases: a dissection (preanhepatic) section, an anhepatic part, and a neohepatic part. Dissection (preanhepatic) part: Through a hockey stick incision, the liver is dissected so that it stays hooked up only by the inferior vena cava and portal vein.
Cheap sustiva 600mg overnight delivery. 24 Signs Someone Likes You More Than Just a Friend.
Changes in systemic capacitance also influence pulmonary blood volume: Systemic venoconstriction shifts blood from the systemic to the pulmonary circulation medications jfk was on discount 200 mg sustiva with visa, whereas vasodilation causes a pulmonaryto-systemic redistribution medications education plans cheap sustiva 600 mg. Hypoxia is a powerful stimulus for pulmonary vasoconstriction (the opposite of its systemic effect) medicine 7 600mg sustiva. Both pulmonary arterial (mixed venous) and alveolar hypoxia induce vasoconstriction medicine 2410 purchase 200 mg sustiva mastercard, but the latter is a extra powerful stimulus. This response appears to be due to both the direct impact of hypoxia on the pulmonary vasculature or elevated manufacturing of leukotrienes relative to vasodilatory prostaglandins. Hypoxic pulmonary vasoconstriction is an important physiological mechanism in decreasing intrapulmonary shunting and preventing hypoxemia. Hypercapnia and acidosis have a constrictor effect, whereas hypocapnia causes pulmonary vasodilation, the other of what happens in the systemic circulation. Regardless of body position, dependent areas of the lung receive larger blood move than nondependent areas. This sample is the outcomes of a gravitational gradient of 1 cm H2O/cm lung height. Also, in vivo perfusion scanning in regular people has proven an "onion-like" layering distribution of perfusion, with lowered move on the periphery of the lung and increased perfusion toward the hilum. In zone 1 (Pa > Pa > Pv), alveolar strain (Pa) is greater than each the arterial pulmonary stress (Pa) and venous pulmonary pressure (Pv), leading to obstruction of blood flow and creation of alveolar dead house. West zone 1 is fairly small in a spontaneously respiration individual, but can enlarge during positive strain ventilation. In dependent areas of the lungs, Pa progressively will increase due to reduced elevation above the center. The bulk of the lung is described by zone 3 (Pa > Pv > Pa), where both Pa and Pv are greater than Pa, leading to blood move independent of the alveolar strain. V/Q for individual lung items (each alveolus and its capillary) can range from zero (no ventilation) to infinity (no perfusion); the previous is referred to as intrapulmonary shunt, whereas the latter constitutes alveolar dead area. Clinically, hypoxemia from a relative 9 Shunting denotes the method whereby desat- A Ventilation Blood circulate B three Blood move and Ventilation V/Q 2 Ventilation 1 Blood move Bottom 0 0. Where Qs = blood flow via the physiologic shunt compartment Qt = total cardiac output Qc = blood move across usually ventilated pulmonary capillaries Qt = Qc + Qs Cco2 = oxygen content of ideal pulmonary end-capillary blood Cao2 = arterial oxygen content material Cvo2 = blended venous content the simplified equation is: Venous Admixture Venous admixture is the amount of combined venous blood that must be mixed with pulmonary end-capillary blood to account for the distinction in O2 pressure between arterial and pulmonary endcapillary blood. Pulmonary end-capillary blood is considered to have the identical concentrations as alveolar fuel. Venous admixture is normally expressed as a fraction of complete cardiac output (Qs/Qt). Qs/Qt could be calculated clinically by acquiring mixed venous and arterial blood gasoline measurements; the former requires a pulmonary artery catheter. Pulmonary capillary blood is normally assumed to be 100 percent saturated for an Fio2 of 0. The calculated venous admixture assumes that every one shunting is intrapulmonary and due to absolute shunts (V/Q = 0). In reality, neither is ever the case; nonetheless, the concept is beneficial clinically. The venous admixture in normal people (physiological shunt) is usually less than 5%. Effects of Anesthesia on Gas Exchange Abnormalities in fuel exchange throughout anesthesia are frequent. Increases in alveolar lifeless area are mostly seen during managed air flow, however can also 10 happen during spontaneous air flow. General anesthesia generally increases venous admixture to 5% to 10%, probably as a result of atelectasis and airway collapse in dependent areas of the lung. Inspired O2 tensions of 30% to 40% usually forestall hypoxemia, suggesting anesthesia increases relative shunt. Prolonged administration of excessive inspired O2 concentrations may be associated with atelectasis formation and will increase in absolute shunt. Atelectasis in this scenario is recognized as resorption atelectasis and seems in areas with a low V/Q ratio ventilated at an O2-inspired focus near 100%. Perfusion results in O2 being transported out of the alveoli at a fee faster than it enters the alveoli, resulting in an emptying of the alveoli and collapse. Oxygen Alveolar Oxygen Tension With every breath, the inspired gasoline combination is humidified at 37�C in the upper airway. In humidified air, the traditional partial strain of O2 at sea level is 150 mm Hg: (760 - 47) � zero. Air has an O2 focus of approximately 21%; subsequently, if the barometric pressure is 760 mm Hg (sea level), the partial stress of O2 (Po2) in air is often 159. Note that large will increase in Paco2 (>75 mm Hg) readily produce hypoxia (Pao2 <60 mm Hg) at room air, however not at excessive impressed O2 concentrations. Pulmonary End-Capillary Oxygen Tension For all practical functions, pulmonary end-capillary O2 rigidity (Pco2) could additionally be thought of equivalent to Pao2; the Pao2�Pco2 gradient is generally minute. Pco2 is dependent on the rate of O2 diffusion throughout the alveolar�capillary membrane, in addition to on pulmonary capillary blood volume and transit time. Enhanced O2 binding to hemoglobin at saturations above 80% additionally augments O2 diffusion (see below). Therefore, pulmonary diffusing capability reflects not only the capacity and permeability of the alveolar�capillary membrane, but also pulmonary blood circulate. Moreover, O2 uptake is normally limited by pulmonary blood move, not O2 diffusion across the alveolar� capillary membrane; the latter might turn out to be important during exercise in regular individuals at excessive altitudes and in patients with intensive destruction of the alveolar�capillary membrane. Low alveolar oxygen rigidity Low impressed oxygen tension Low fractional impressed concentration High altitude Alveolar hypoventilation Diffusion hypoxia Increased oxygen consumption Increased alveolar�arterial gradient Right-to-left shunting Increased areas of low V/Q1 ratios Low mixed venous oxygen rigidity Decreased cardiac output Increased oxygen consumption Decreased hemoglobin focus 1 V, ventilation/perfusion. Such impediments may be due to abnormal V/Q ratios, intensive destruction of the fuel alveolar� capillary membrane, or very quick capillary transit instances. Abnormalities are accentuated by increases in O2 consumption and cardiac output, similar to occurs during train. The alveolar-to-arterial O2 partial strain gradient (A�a gradient) is generally the range is 60 to a hundred mm Hg. The commonest mechanism for hypoxemia is an elevated alveolar�arterial gradient. The A�a gradient for O2 depends on the quantity of right to-left shunting, the amount of V/Q scatter, and the combined venous O2 rigidity (see below). The A�a gradient for O2 is directly proportional to shunt, however inversely proportional to combined venous O2 rigidity. The impact of each variable on Pao2 (and consequently the A�a gradient) can be determined only when the opposite variables are held fixed. It must also be famous that the higher the shunt, the much less likely the likelihood that an increase in Fio2 will correct hypoxemia. Moreover, isoshunt strains seem to be most useful for O2 concentrations between 35% and 100 percent. Lower O2 concentrations require modification of isoshunt lines to account for the impact of V/Q scatter. A discount in venous admixture may be observed with low-normal cardiac outputs secondary to accentuated pulmonary vasoconstriction from a lower blended venous O2 rigidity. On the other hand, excessive cardiac outputs can improve venous admixture by elevating mixed venous O2 rigidity, which in turn inhibits hypoxic pulmonary vasoconstriction. O2 consumption and hemoglobin concentration can even have an effect on Pao2 via their secondary results on mixed venous O2 tension (below). High O2 consumption charges and low hemoglobin concentrations can enhance the A�a gradient and depress Pao2. A true blended venous blood sample incorporates venous drainage from the superior vena cava, the inferior vena cava, and the heart; it should therefore be obtained from a pulmonary artery catheter. As may be seen, a low Carbon dioxide is a by product of cardio metabolism in mitochondria. During periods of acute hypoventilation or hypoperfusion, body content material of carbon dioxide will increase. Oxygen O2 is carried in blood in two types: dissolved in answer and in reversible association with hemoglobin. Hemoglobin saturation is the amount of O2 certain as a percentage of its complete O2-binding capability. Four separate chemical reactions are concerned in binding each of the four O2 molecules. The change in molecular conformation induced by the binding of the primary three molecules greatly accelerates binding of the fourth O2 molecule.