V-gel
| Contato
Página Inicial
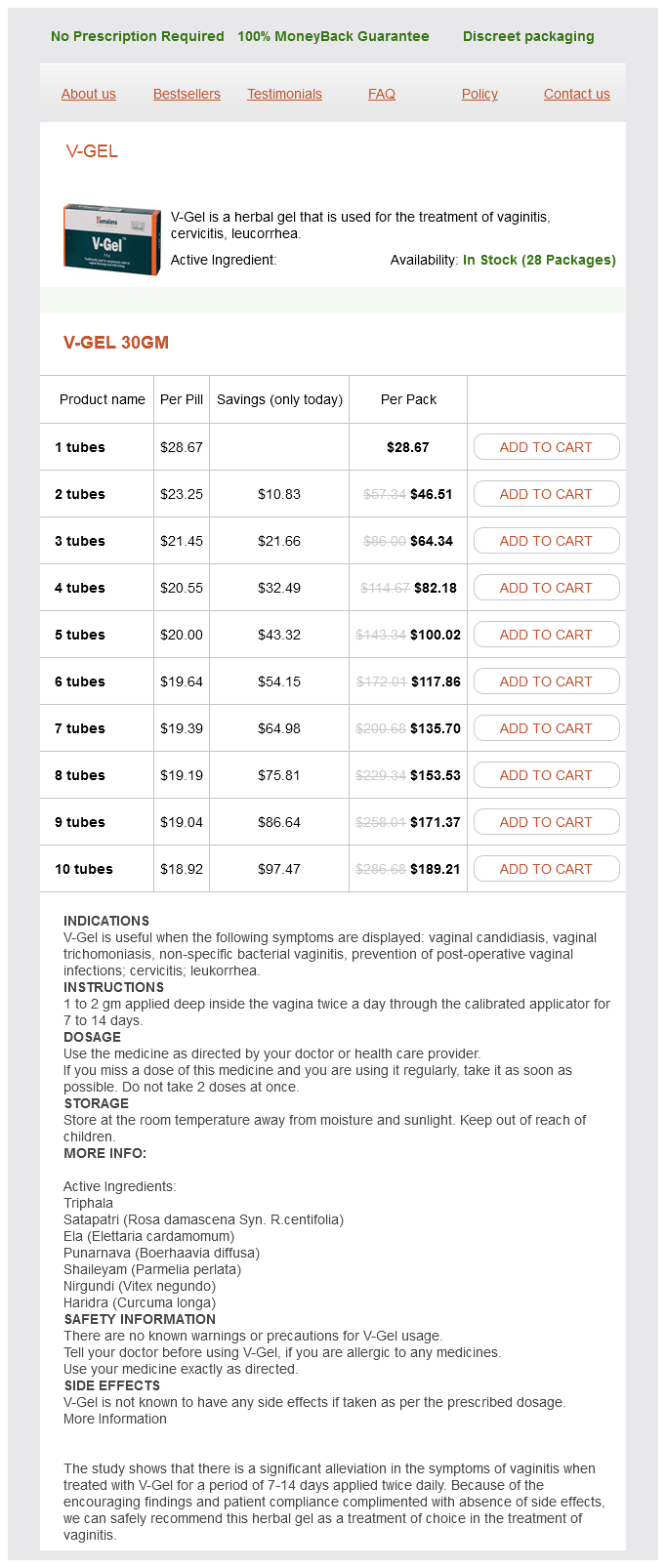
"Order v-gel 30 gm on-line, herbs names".
W. Mortis, M.B. B.CH. B.A.O., Ph.D.
Assistant Professor, Yale School of Medicine
Repair of a tongue laceration in any patient is tough herbals detox v-gel 30 gm generic line, however in an uncooperative youngster herbs de provence walmart 30 gm v-gel purchase fast delivery, the process could show inconceivable with out basic anesthesia herbals on deck review 30 gm v-gel cheap fast delivery. Anesthetize a localized space of the tongue topically by masking the world with 4% lidocaine-soaked gauze for 5 minutes herbals stock photos v-gel 30 gm. Determine the maximum protected dose of native anesthetic and keep away from exposure to greater doses. Large lacerations require infiltration anesthesia (1% lidocaine with buffered epinephrine) or a lingual nerve block. If the tip of the tongue has been anesthetized, a towel clip or suture can be used to maintain protrusion of the tongue in an uncooperative affected person. Further anesthesia and subsequent wound cleansing and closure are possible whereas an assistant applies light traction on the tongue. Blood vessels in the fascia are the main source of the bleeding in scalp lacerations. Scalp Lacerations the scalp extends from the supraorbital ridges anteriorly to the external occipital protuberances posteriorly and blends with the temporalis fascia laterally. The scalp has 5 anatomic layers: pores and skin, superficial fascia, galea aponeurotica, subaponeurotic areolar connective tissue, and periosteum. The outer layer consists of the pores and skin, superficial fascia, and galea (the aponeurosis of the frontalis and occipitalis muscles), which are firmly adherent and surgically thought-about as one layer. The integrity of the outer layer is maintained by inelastic, tough, fibrous septa, which maintain wounds from gaping open until all three parts have been traversed. The galea itself is loosely adherent to the periosteum by means of the slack areolar tissue of the subaponeurotic layer. Stellate lacerations are frequent on this area, not solely because the scalp is vulnerable to blunt trauma but in addition because its superficial fascial layer is inelastic and firmly adherent to the pores and skin. Stellate lacerations pose additional technical problems in closure and have a greater propensity for an infection. Debris and other contaminants may be deposited several centimeters from the visible laceration; due to this fact, cautious exploration plus cleansing of scalp wounds is essential. When scalp wounds are d�brided, clearly devitalized tissue ought to be removed, however d�bridement must be conservative as a result of closure of large defects on the scalp is troublesome. The presence of a rich vascular network in the superficial fascia leads to profuse bleeding from scalp wounds. The subgaleal layer of loose connective tissue incorporates emissary veins that drain through diploic vessels of the skull into the venous sinuses of the cranial hemispheres. In scalp wounds that penetrate this layer, bacteria may be carried by these vessels to the meninges and the intracranial sinuses. Thus, a scalp wound infection can end result in osteomyelitis, meningitis, or a brain abscess. Profuse bleeding, especially from intensive scalp lacerations, is finest controlled by suturing130 (see also Chapter 34). Ask an assistant to maintain compression around the wound when you full closure of the wound. A simple process that often provides hemostasis of scalp wounds is to place a wide, tight rubber band or Penrose drain across the scalp from the forehead to the occiput. You can even control bleeding temporarily in some cases by greedy the galea and the dermis with a hemostat and everting the instrument over the edge of the skin. The drawback of this method is that tissue grasped by the hemostat may be crushed and devitalized. If bleeding from the sting of the scalp wound is vigorous and definitive restore must be postponed whereas the patient is resuscitated, Raney scalp clips or a hemostat could be utilized rapidly to the sting of the scalp wound to management the hemorrhage. Before wound closure, visually look at the underlying skull and palpate it for skull fractures. However, a common error is to mistake a tear in the galea or the periosteum for a fracture throughout palpation contained in the wound. Of particular importance are stab or puncture wounds within the scalp and brow, corresponding to from a nail, spike, screwdriver, knife, or ice pick. Without a laceration to explore, such wounds could appear benign, and the patient can initially seem relatively asymptomatic, yet the cranium or mind has been penetrated. When evaluating a puncture or stab wound to the top, a computed tomography scan might present unexpected findings of a cranium fracture, linear or depressed, or an underlying brain harm or early hemorrhage. B, Puncture wounds in the forehead and scalp from such objects as a knife, nail, screwdriver, or ice choose can penetrate the cranium and brain, and initially the affected person appears nicely and the wound looks benign. As said in different sections, avoid shaving, and instead clip hair to keep away from additional harm. Because of the extensive collateral blood supply of the scalp, most lacerations in this space heal with out drawback, even after delayed therapy. Nonetheless, wound cleaning must be adequate to avoid the devastating complication of scalp infection. With microvascular methods, massive sections of skin avulsed from the scalp can be reimplanted. Some of those similar methods are used to salvage avulsed scalp, much like these used for amputated extremities. Separate closure of the galea introduces extra suture materials into the wound and will increase the danger for an infection. However, in extremely large wounds, separate closure could also be necessary to present a more secure approximation of the galea than can be obtained with a large-needle, single-layer closure. In this case, an inverted stitch (with an absorbable 3-0 or 4-0 suture) will bury the knot beneath the galea. Avoid smaller suture materials because it tends to break when agency knots are being tied. Leave the ends of the tied scalp sutures no less than 2 cm long to facilitate subsequent removal. Absorbable sutures might present related beauty and useful outcomes in scalp laceration repair. Place gauze sponges over the laceration to present direct local strain beneath the elastic bandage. Advantages of this technique embody beauty outcomes similar to suturing, increased speed of restore, no want for clipping of hair, and no want for return visit for suture or staple elimination. To close a scalp laceration that extends via the galea, use a long needle, forceps, and 3-0 sutures (blue polypropelene sutures make removal easier). The affected person must be informed that the glue will gradually fall off within two weeks. If the drop of glue fails to fall off, it could be merely eliminated with tweezers or comb. Nail Bed Lacerations Injuries to the nail and nail bed (also called the nail matrix) are frequent problems in emergency medicine, but controversy exists over correct management. Some nail mattress lacerations are minor and of no consequence, whereas others portend a poor consequence unless the bed is repaired. Suture the nail mattress if a large subungual hematoma is associated with an unstable or avulsed nail. A good consequence is determined by maintaining the space under the eponychium (cuticle) because the laceration heals and the model new nail grows out, which is a sluggish process. Prohibiting bathing with sutures in place in any a part of the body has no scientific benefit. Partial Nail Avulsions If the nail is partly avulsed (especially at the base) or unfastened, raise the nail to assess and potentially repair the nail bed. Repeat, every 1�2 cm alongside the wound, bisecting the wound simply as if utilizing sutures. B, from Karaduman S, Yurukrumen A, Guryay S, et al: Modified hair apposition technique as the primary closure methodology for scalp lacerations, Am J Emerg Med 27:1050, 2009. The distal finish of the nail covers the sterile matrix; the proximal finish arises from and covers the germinal matrix. The tissue adherent to the proximal dorsal floor of the nail is the eponychium (also termed the cuticle), and the potential space between the nail and the eponychium is the nail fold. Even though a nail matrix laceration (the supply of the bleeding) is present, the beauty end result might be wonderful. All blood must be drained within the emergency department before discharge to guarantee correct therapy. Compare it with A, the place no blood is seen within the paronychial space because the nail base remains intact.
These three nerves arise from the lumbar plexus and travel proximally inside the identical fascial compartment herbals for ed discount 30 gm v-gel free shipping. The 3-in-1 block proceeds as described beforehand herbs de provence uses v-gel 30 gm sale, but utilizes a volume of 20 to 30 cc of medicine kan herbals v-gel 30 gm discount. To carry out the fascia iliaca block using ultrasound guidance jeevan herbals order 30 gm v-gel free shipping, insert the needle in-plane simply inferior to the inguinal ligament and information it underneath the fascia iliaca, which lies simply superior to the vessels. The tibial and common peroneal nerves may be blocked within the popliteal fossa to present anesthesia to the distal part of the calf, ankle, and foot. Both are simply recognized within the popliteal fossa, where they exist as separate structures. The transducer ought to be positioned transversely within the popliteal fossa, and the popliteal artery should be sought. Once the artery has been identified, the tibial nerve can be discovered slightly superficial ("excessive and out of doors") to the artery. As with other peripheral nerves, the tibial nerve seems as an echogenic, rounded structure. The peroneal nerve (arrow) is often slightly more superficial than the tibial nerve (arrowhead). Once each nerves have been recognized, apply anesthetic beneath direct ultrasound steering as described earlier. The popliteal vein could be seen just under the nerve and serves as a landmark for locating the nerve. As with upper extremity nerve blocks, notice any neural or vascular accidents earlier than the injection. Deficits, even if questionable, ought to be documented within the report and delivered to the eye of the patient earlier than performance of the nerve block. Markham A, Faulds D: Ropivacaine: a evaluation of its pharmacology and therapeutic use in regional anaesthesia. Liebmann O, Price D, Mills C, et al: Feasibility of forearm ultrasonographyguided nerve blocks of the radial, ulnar, and median nerves for hand procedures in the emergency department. Selander D, Dhuner Kg, Lundberg g: Peripheral nerve harm due to injection needles used for regional anesthesia. Blaivas M, Adhikari S, Lander L: A prospective comparison of procedural Sedation and ultrasound-guided Interscalene nerve block for shoulder discount within the emergency division. Sehmbi H, Shah U, Madjdpour C, et al: Ultrasound guided distal peripheral nerve block of the upper limb: a technical evaluate. Sohoni A, Nagdev A, Takhar S, et al: Forearm ultrasound-guided nerve blocks vs landmark-based wrist blocks for hand anesthesia in healthy volunteers. Knoop K, Trott A, Syverud S: Comparison of digital versus metacarpal blocks for repair of finger injuries. Ellis gL, Owens A: the efficacy and acceptability of utilizing a jet injector in performing digital blocks. Dickman E, Pushkar I, Likourezos A, et al: Ultrasound-guided nerve blocks for intracapsular and extracapsular hip fractures. Marhofer P, Nasel C, Sitzwohl C, et al: Magnetic resonance imaging of the distribution of local anesthetic during the three-in-one block. Chesters A, Atkinson P: Fascia iliaca block for ache relief from proximal femoral fracture in the emergency department: a evaluation of the literature. However, the Bier block has now gained broad acceptance as a secure and effective procedure, and several papers extol its virtues. Though traditionally relegated to the operating room, the procedure can be readily relevant to outpatient use. The procedure is free from the troublesome side effects related to other regional blocks, such as the axillary block. The procedure is definitely mastered and has a really low failure fee; constantly good outcomes could be expected. The process could additionally be carried out on any affected person of any age who is ready to cooperate with the clinician. The solely absolute contraindications are allergy to the anesthetic agent and, probably, uncontrolled hypertension. Homozygous sickle cell disease is a theoretical contraindication, however few information exist on the therapy of patients with this condition. The only painful portions of the *Commercial preparations with preservatives are commonly used. While the patient is being ready, hold the lidocaine answer ready, however withhold it till the injured extremity is exsanguinated and the cuff is in place and inflated, as discussed later. Hence, for a 70-kg affected person, infuse 210 mg of lidocaine (21 mL of 1% lidocaine) blended with 21 mL of saline for a complete quantity in the infusing syringe of 42 mL of 0. Farrell and coworkers described a procedure termed the minidose Bier block in which 1. Apply a pneumatic tourniquet with cotton padding (to stop ecchymosis) underneath the cuff proximal to the pathology. A specially designed portable double-cuff pneumatic system, similar to that marketed by Zimmer Corporation, is good and most popular by the writer. Inflate the tourniquet and place a plastic catheter or a metal butterfly needle in a superficial vein as close to the pathologic web site as potential, and securely tape it in place. It is usually desirable to use a vein on the dorsum of the hand, but importantly, the injection web site ought to be no much less than 10 cm distal to the tourniquet to keep away from injection of anesthetic proximal to or under the tourniquet. Keep the hub on the catheter to keep away from backbleeding, or connect the syringe to the butterfly tubing. Anesthesia from a fingertip-to-elbow path appears to happen regardless of the site of infusion of the anesthetic, but selecting an injection location near the site of pathology might present extra rapid anesthesia at a lower dosage. Simple elevation of the extremity for a couple of minutes could additionally be enough, but wrapping the extremity in a distal-to-proximal path with an elastic or Esmarch bandage, while being cautious to not dislodge the infusion needle, significantly enhances exsanguination. Wrapping may be painful, so this step may be eliminated if it causes too much anxiousness for the affected person. During the wrapping process, take care to not dislodge or infiltrate the infusion catheter. With the extremity still elevated or wrapped, inflate the tourniquet to 250 mm Hg (or a hundred mm Hg above systolic pressure). In elderly overweight sufferers with calcified peripheral vessels, arterial occlusion is in all probability not achieved safely. In three to 5 minutes, the patient will expertise paresthesia or warmth beginning within the fingertips and touring proximally, with last anesthesia occurring above the elbow, to the extent of the tourniquet. Note that enough analgesia might exist even when the patient can still sense touch and position and has some motor perform. Additional lidocaine was required in 7% of circumstances in a single series by which the minidose routine was used. Alternatively, if analgesia is slow or insufficient, an additional 10 to 20 mL of saline solution could also be injected to complement the whole quantity of solution to improve the impact. For overweight sufferers, a most of 300 mg of lidocaine is suggested for the arm and not extra than four hundred mg for the leg. Next, withdraw the infusing needle and tightly tape the puncture website to stop extravasation of the anesthetic agent. Perform the surgical procedure or manipulation, including postreduction x-ray films and casting or bandaging. On completion of the procedure, deflation of the tourniquet may be cycled to stop a bolus impact of any lidocaine that will stay in the intravascular compartment. This might be required provided that the cuff has been inflated for lower than 30 minutes. A single deflation is usually carried out if the cuff has been inflated for longer than this time. If the tourniquet has been in place for less than 30 minutes, a rise in transient lidocaine-related side effects may be seen if cycled deflation has not been used because enough tissue fixation of the lidocaine has in all probability not occurred. This may lead to a higher peak plasma lidocaine stage, with increased unwanted aspect effects. Sensation returns shortly when the tourniquet is eliminated, and in 5 to 10 minutes the extremity returns to its pre-anesthetic level of sensation and performance. Many sufferers describe a transient intense tingling sensation after cuff deflation. A extensive tourniquet cuff (14 cm) is less painful than a slender tourniquet (7 cm) when the cuff is inflated 10 mm Hg above lack of the arterial pulse.
If spontaneous discount occurs before analysis in the emergency division herbals on demand shipping cheap v-gel 30 gm, this prognosis could not even be thought-about aasha herbals - v-gel 30 gm cheap line. Arterial injury (especially popliteal artery) is a severe complication of a knee dislocation herbs pregnancy 30 gm v-gel generic mastercard. An arteriogram is the gold normal for evaluation of arterial injuries herbs thai bistro order v-gel 30 gm on line, which may initially be delicate or delayed. However, knee dislocation has been reported after minor mechanisms, similar to stepping off a curb or into a gap, normally in affiliation with a twisting action. These sufferers are extra commonly ladies and are at increased risk of vascular harm when in comparability with high-energy mechanism multi-ligament disruptions. Rotatory dislocations may be anteromedial, anterolateral, posterolateral, or posteromedial. When a spontaneously decreased knee dislocation is related to different major trauma, the diagnosis may be missed. Obese patients could have a seemingly regular look of their knee, but an apparent deformity might be seen on the preliminary radiographs. An spectacular effusion is most likely not present with a knee dislocation as a outcome of the joint capsule is commonly disrupted and extravasation occurs into the encompassing tissue, often posteriorly. The most necessary a half of the clinical assessment is the vascular standing of the extremity (see the following section). Nerve injury is much less widespread, however peroneal nerve damage is a acknowledged complication, particularly with a posterolateral dislocation. Posterolateral dislocations could additionally be irreducible as a result of the medial femoral condyle buttonholes through the joint capsule. Vascular Injury the most feared complication of a knee dislocation is severance or internal injury of the popliteal artery. The incidence of popliteal artery damage in a dislocated knee is approximately 20% in most series. Varnell and associates138 reported a pulse deficit or absent pulse in all patients with vascular injury. Kendall and coworkers139 additionally reported clear clinical evidence of all popliteal artery injuries in knee dislocations. This group recommended exploration for obvious ischemia, angiography for sufferers with ischemia whose pulse is restored after relocation, and remark for all others. Miranda and associates148 reported that popliteal artery harm can be safely and reliably predicted by a bodily examination that includes specific analysis for lively posterior hemorrhage (expanding hematoma, absent pulse, or the presence of a thrill or bruit). Thus, though centered clinician examination could also be quite accurate in the vast majority of circumstances, any dislocated knee ought to prompt critical concern in regards to the vascular integrity of the leg given the sometimes refined or delayed manifestation of vascular accidents. Simple palpation of the artery may not be sensitive enough to detect a decreased pulse. In addition, think about digit pulse oximetry to compare the uninjured leg with the injured one. No patient on this group was discovered to have vascular compromise at follow-up (range, 4 to 36 months). Internal derangement with a knee hemarthrosis (often of the dimensions noted with a torn anterior cruciate ligament) is a typical first sign that the knee had beforehand been dislocated and spontaneously reduced. Therefore all knee injuries with significant swelling, hemarthrosis, or a dislocating mechanism of harm should be evaluated with the precise intent of ruling out vascular damage. Early consultation ought to be searched for knee dislocations because of the excessive incidence of problems and the frequent need for operative intervention. The choice to pursue angiography in a patient with a dislocated knee is best made in session with an orthopedic surgeon. The basic initial approach for every type of knee dislocation is to apply traction to the extremity. This Knee Dislocation Reduction 3 1 2 Additional maneuvers may be required, relying on the sort of dislocation. Often this maneuver alone will cut back the joint because of the extreme ligamentous disruption related to the dislocation. The interosseous distance is widened and the proximal end of the fibula is displaced laterally. For posterior dislocations, carry the proximal end of the tibia to full the reduction. It is accompanied by apparent prominence of the fibular head anteriorly; no associated neurovascular issues are noted. The less frequent posterior dislocation could additionally be accompanied by peroneal nerve injury. These injuries trigger extreme ligamentous and other derangements within the knee and generally require operative stabilization with a long interval of recovery and physical therapy. Reduction Technique To scale back an anterior fibular head dislocation, place the patient supine and flex the affected knee to 90 degrees to chill out the biceps femoris tendon. Dorsiflex and externally rotate the foot and apply direct stress to the fibular head; discount is often signified by a snap. When the knee is flexed, the soundness of this joint is decreased because of leisure of the fibular collateral ligament. The ordinary mechanism is a powerful quadriceps contraction mixed with a powerful valgus and external rotation element. The affected person will report that the leg "went out" and will describe truly seeing the lateral deformity attributable to the displaced patella. Clinical clues to a spontaneously lowered patella include the presence of a knee effusion and tenderness alongside the medial fringe of the patella. Osteochondral fractures are detectable in roughly half the patients with patellar dislocations, but many of these fractures are seen only on arthroscopy. The medical prognosis of patellar dislocation in an older patient ought to be made with caution as a end result of these are primarily injuries involving the young. C Superior dislocation Lateral view D Intercondylar dislocation Lateral view Reduction Technique and Post-Reduction Care Reduction of a lateral patellar dislocation is often quite simple. If the affected person is anxious or in great discomfort, premedication must be considered (see Chapter 33). The two basic maneuvers for patellar relocation are extension of the knee and mild medial stress applied to the patella whereas lifting essentially the most lateral fringe of the patella over the femoral condyle. Orthopedic follow-up is necessary because of the need for bodily remedy and the excessive fee of persistent instability. Recurrent dislocations and people associated with an osteochondral fracture might require operative restore. Patellar dislocations in different locations are often irreducible, and orthopedic session should be sought. Intracondylar, superior, and vertical axis (dorsal fin) dislocations are extraordinarily rare and require operative reduction. The uncommon horizontal dislocation may relocate with closed discount, however surgical reduction is usually necessary. The knee is held in flexion, and the patella (arrow) may be seen and palpated along the lateral facet of the knee. Posterior dislocations of the ankle are extra frequent than anterior dislocations, they usually normally end result from a fall on a plantar-flexed foot. Patients with posterior dislocations usually Clinical Assessment lateral dislocation of the patella is mostly clinically obvious. The knee is held in a point of flexion and the patella can easily be seen and palpated on the lateral side of the knee. Tenting of the patella is often detectable until significant delicate tissue swelling is present. Anterior dislocations typically result from pressured dorsiflexion or a blow directed posteriorly onto the distal end of the tibia whereas the foot is fastened. The talus is outstanding anteriorly, and the dorsalis pedis pulse may be misplaced secondary to strain from the talus. Superior dislocations are uncommon and end in diastasis of the tibiofibular joint. These injuries are often the end result of a significant axial pressure, such as a fall from a major top. Therefore clinicians ought to search for concomitant calcaneal or low backbone fractures. Radiographic Examination Because of the high price of associated fractures and the medical problem in assessing for the presence or the exact nature of a dislocation, it is strongly recommended that pre-reduction radiographs be obtained for all suspected ankle dislocations. The emergency clinician will typically have to scale back these injuries because of the extreme lateral deformity and occasional compromise of the dorsalis pedis artery by stretch.
Under no circumstances ought to a nonintubated patient bear lavage within the restrained supine position zeolite herbals pvt ltd cheap v-gel 30 gm fast delivery. Smaller lotus herbals 3 in 1 matte review v-gel 30 gm order otc, more flexible tubes could kink and are considerably harder to pass herbals teas safe during pregnancy 30 gm v-gel cheap with visa. In most instances herbs unlimited v-gel 30 gm generic with mastercard, a 36- to 40-Fr or a 30-English gauge tube (external diameter, 12 to thirteen. Passage of an extreme size of hose might trigger gastric distention, bruising, and perforation, whereas passage of an inadequate length of hose may lead to lavage of the esophagus and elevated threat for emesis and aspiration. Commercial lavage techniques are available and often use either a gravity fill-and-empty system with a Y-connector or a closed irrigation syringe system. Alternatively, an irrigation syringe can be utilized for intermittent input and withdrawal of lavage fluid. Technique lubricate the gastric tube and cross it gently to avoid harm to the posterior pharynx. Use of a bite block or an oral airway may forestall the patient from chewing on the orogastric tube and biting the fingers of the inserter. Cough, stridor, or cyanosis signifies that the tube has entered the trachea; withdraw the tube instantly and reattempt passage. Intragastric placement is normally evident on clinical grounds by the spontaneous egress of gastric contents however could additionally be confirmed by auscultation of the stomach throughout injection of air with a 50-ml syringe followed by successful aspiration of gastric contents. However, due to the risk of lavage via a misplaced tube, affirm tube place radiographically earlier than lavage is carried out. A misplaced tube could irrigate the esophagus with a tube that has doubled again on itself during passage. The most critical complication, aside from esophageal perforation, is inadvertent passage of the tube into the lungs. Tracheal passage of a lavage tube must be readily apparent in an awake affected person before lavage, and obtunded patients are intubated, thereby obviating this problem. If an awake affected person begins to vomit during lavage, instantly remove the tube to permit the affected person to defend the airway. With the Y-connector closed system, carry out lavage by clamping the drainage arm of the Y-adapter and infusing aliquots of fluid into the stomach from a reservoir. Clamp the reservoir arm of the Y, and then open the drainage arm to permit drainage of the stomach contents by gravity. Apply suction intermittently to the drainage tubing to enhance emptying of the abdomen. Because electrolyte disturbances have occurred in youngsters who underwent lavage with faucet water, prewarmed (45�C) regular saline is generally really helpful for children. Use a chunk block or an oral airway to forestall the patient from biting the tube or inserter. Before gastric irrigation, remove the gastric contents by careful gastric aspiration with repeated repositioning of the tip of the tube. After gastric aspiration and lavage are completed, administer a slurry of activated charcoal through the gastric tube. In an awake affected person the orogastric tube could be handed with the patient within the sitting position, however the lavage procedure is finest performed with the affected person within the left lateral decubitus place. B, the left lateral decubitus place is preferred for lavage to isolate the gastric contents and avoid reflux. Extra holes may be reduce in the aspect of the tube to facilitate the elimination of large fragments. After gastric aspiration and lavage have been completed, administer a slurry of activated charcoal through the gastric tube. When now not needed, clamp off the gastric tube before removing to avoid "dribbling" fluid into the airway. Some pediatric textbooks suggest a 24-Fr oral gastric tube for toddlers and a 36-Fr tube for adolescents. Some would recommend an oral route for this tube, but it was passed rather simply via the nose. Although lavage could have been cheap in this state of affairs, a potent and secure antidote for digoxin does exist. Thompson and co-workers reported that in lavage 36% of patients had atrial or ventricular ectopy, 4. The great amount of fluid administered throughout lavage has been reported to cause fluid and electrolyte disturbances. These disturbances have been seen with the utilization of each hypertonic and hypotonic lavage fluid in the pediatric inhabitants. Pulmonary aspiration of gastric contents or lavage fluid is the primary potential danger during gastric lavage, especially in patients with compromised protective airway reflexes. Kinking or knotting of the tube can occur, however sometimes a tube might become stuck because of decrease esophageal spasm. If neither fluoroscopy nor radiography demonstrates deformation of the lavage tube, 1 to 2 mg of intravenous glucagon can be infused in an try to relieve lower esophageal spasm. Use of Endoscopy to Perform Gastric Lavage the technique of gastric lavage can also be completed utilizing an endoscopic approach. Bezoar formation might occur with overdoses of a massive quantity of tablets or certain types of brokers. There are numerous case reviews of bezoar formation following acute overdose, with subsequent endoscopic removal and clinical improvement. Because the massive gastric tube is irritating and will predispose the patient to gagging, drooling, or aspiration, it ought to be eliminated. Complications A correctly performed procedure in the appropriate surroundings is usually protected, however quite a few issues have been associated with gastric lavage. Depending on the route selected for insertion of the tube, injury to the nasal mucosa, turbinates, pharynx, esophagus, and abdomen has been reported. Scalzo and associates found radiographically that 7 of 14 kids had improper tube placement (too high or too low) regardless of optimistic gastric auscultation in all instances. The use of activated charcoal for poisoning has been recognized for nearly two centuries. To reveal the effectiveness of charcoal, in 1930, French pharmacist Touery ingested a number of times the deadly dose of strychnine combined with 15 g of activated charcoal. He performed this act in front of a class of colleagues and exhibited no sick effects. Activated charcoal acts each by adsorbing a variety of poisons current in the gastrointestinal tract and by enhancing elimination of toxins if systemic absorption has already occurred. It enhances elimination by creating a concentration gradient between the contents of the bowel and the circulation, nevertheless it also has the potential to interrupt enterohepatic circulation if the actual toxin is secreted in bile and enters the gastrointestinal tract before reabsorption. It can be seen descending below the diaphragm (1), and the interruption in the radiopaque line (which signifies essentially the most proximal hole) is in the stomach (2). The tube could be seen descending beneath the diaphragm (1) but is kinked in the abdomen (2) and has doubled again on itself. The hole within the radiopaque line (3) is on the level of the gastroesophageal junction, and the distal tip of the tube is in the midesophagus (4). Proper measurement of the tube earlier than insertion would in all probability have prevented this misplacement. Indications For years, administration of a single oral dose of activated charcoal for essentially all overdoses was routine. However, with the emergence of latest tips in overdose management43 the usage of charcoal declined to lower than 1% of poisoned patients in 2014. This will normally be a medical determination because sufficient historic data could often be missing. It can also be administered by multiple dosing if the clinician anticipates that the charcoal will end in elevated clearance of an already absorbed drug. Because the contents could settle with time, shake the bottle vigorously earlier than administration. The adsorptive capability of charcoal depends on the inherent properties of the toxin and the native milieu, corresponding to pH. Adsorption begins within minutes of contact with a toxin but might not attain equilibrium for 20 to half-hour. Based on volunteer studies, the effectiveness of activated charcoal decreases with time; the greatest profit is inside 1 hour of ingestion. The administration of activated charcoal could additionally be thought of if a affected person has ingested a probably toxic quantity of a poison (which is known to be adsorbed to charcoal) as much as 1 hour previously; there are insufficient data to assist or exclude its use after 1 hour of ingestion.
V-gel 30 gm order otc. How I cured myself of chronic illness and reversed ageing | Darryl D'Souza | TEDxPanaji.