
Viagra Professional
| Contato
Página Inicial
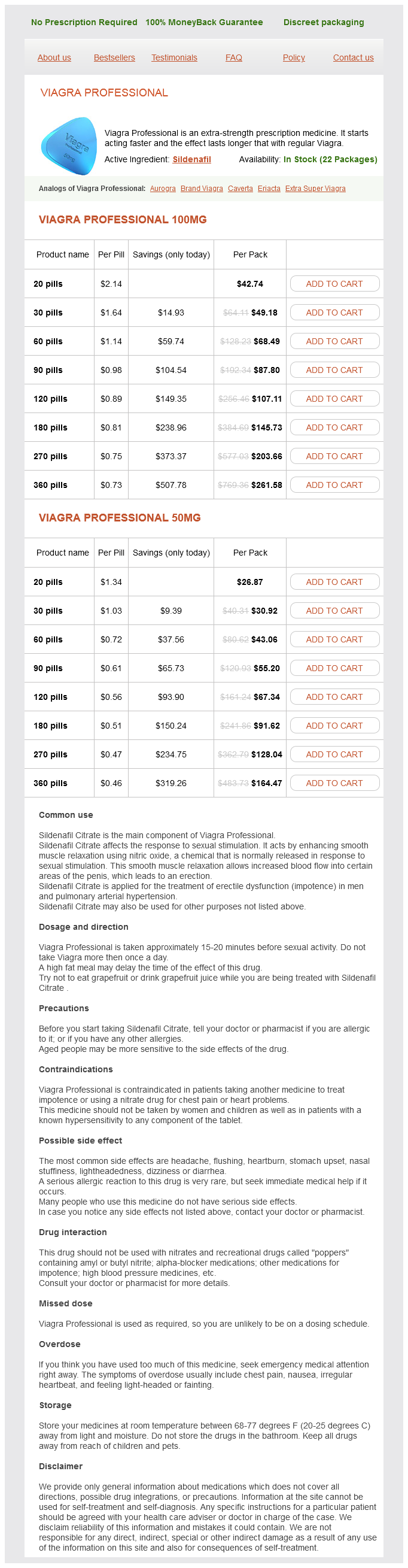
"50 mg viagra professional generic visa, erectile dysfunction muse".
D. Nefarius, M.B.A., M.B.B.S., M.H.S.
Vice Chair, Campbell University School of Osteopathic Medicine
The impact of fusion on adjacent levels in cervical backbone accidents: Is it actually essential Adjacent stage ossification development after anterior cervical fusion with out plate fixation erectile dysfunction injections treatment cheap viagra professional 100 mg fast delivery. Biomechanical research on the impact of cervical spine fusion on adjacent-level intradiscal stress and segmental movement injections for erectile dysfunction side effects viagra professional 100 mg purchase mastercard. Clinical outcomes and growth of heterotopic ossification in complete cervical disc replacement throughout a 4-year follow-up impotence due to diabetes buy cheap viagra professional 50 mg online. An analysis of heterotopic ossification in cervical disc arthroplasty: a novel morphologic classification of an ossified mass icd 9 code for erectile dysfunction due to diabetes 50 mg viagra professional with mastercard. Analysis of the incidence and medical effect of the heterotopic ossification in a single-level cervical synthetic disc substitute. The predisposing components for the heterotopic ossification after cervical artificial disc alternative. Double-level cervical complete disc substitute for adjoining phase illness: is it a useful treatment Failure of Anterior Cervical, Low-Profile, Stand-Alone Screw�Plate Devices 18 Failure of Anterior Cervical, Low-Profile, Stand-Alone Screw�Plate Devices Michael P. Patient variables related to postoperative dysphagia include gender, age, and the presence of prior anterior cervical surgeries. Of these checks, patient-reported consequence scores are doubtless the most specific to a clinically relevant dysphagia. As anterior cervical plating is a variable modifiable by the surgeon, interest in alternative strategies of rigid instrumentation, without plating, has grown and has led to the development of low-profile, stand-alone gadgets. In addition to these fusion devices, cervical disc arthroplasty is one other know-how that permits for low-profile instrumentation and will scale back postoperative dysphagia. Stand-alone, low-profile cervical units have been designed to permit rigid fixation of the adjoining stage, with out requiring the removal of instrumentation above or beneath the pathologic segment. Further sagittal plane correction is obtained by way of positioning, Smith�Petersen osteotomies, and compression via posterior instrumentation. If one locations screws into each the cranial and caudal endplates, the sagittal airplane is locked and no further correction is feasible. This method exploits the aircraft between the sternocleidomastoid and the medial strap muscles. This mobilizes the strap muscular tissues and different neck contents greater than a confined strategy, decreasing stretch and pressure on the muscle tissue. If one chooses not to sacrifice the omohyoid, then it should be retracted medially at C5 and above, laterally when under C5. This lack of stability on the bone�implant interface, we imagine, raises the danger for pseudarthrosis. This is additional complicated by the design as a end result of most have a comparatively small lumen and this lumen is, partly, occupied by the screws used to fix the system. This muscle must be dissected off in a subperiosteal trend, shifting distal to proximal. However, one must observe the quantity of creep upon the adjacent disc area by the plate. He introduced with persistent pain and worsening symptoms; workup revealed pseudarthrosis. Plan was low-profile, standalone system at C4�C5, without removal of instrumentation. If intraoperative, neurophysiologic monitoring is used, the neurophysiologist ought to know when screws are positioned to guarantee no data adjustments ensue. It has been shown to be most frequent when anterior plates are placed inside 5 mm of the adjacent disc area. Despite this potential profit, dysphagia is common and may be minimized with surgical approach through the publicity. Note the cranial creep of the prior instrumentation makes applicable angulation of the cranial screw inconceivable. She was handled with elimination of instrumentation and anterior cervical discectomy and fusion, with anterior plating. This is particularly true of revision procedures, the place scar tissue might act as an obstacle to a wide exposure. Low-profile, stand-alone cervical instrumentation might lower postoperative dysphagia, though other variables, together with age, gender, and ranges treated, are related to dysphagia as nicely. Careful surgical planning and performance will decrease the chance of problems following any anterior cervical procedure. Anterior cervical discectomy and fusion with a zero-profile integrated plate and spacer gadget: a scientific and radiological examine: clinical article. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: a 5to 11-year follow-up research. Comparison of dysphagia between cervical synthetic disc substitute and fusion: information from a randomized controlled research with two years of follow-up. Surgical anatomy of the cervical sympathetic trunk throughout anterolateral method to cervical spine. Vertebral artery anatomy: a evaluate of 2 hundred fifty magnetic resonance imaging scans. Integrated intervertebral gadget for anterior cervical fusion: an initial experience. The scientific efficacy of shortterm steroid remedy in multilevel anterior cervical arthrodesis. Effect of retropharyngeal steroid on prevertebral soft tissue swelling following anterior cervical discectomy and fusion: a prospective, randomized research. The prevalence of cervical myelopathy increases with age from roughly 13% within the third decade of life to practically 100% by the age of 70 years. Removal of the central vertebral body permits for satisfactory decompression of the spinal cord. While halo vests could also be an efficient means of immobilization in sure scientific scenarios, their use is associated with discomfort as nicely as minor and main problems for the patient. Given the excessive failure rates of multilevel anterior fusions, the use of anterior plating was prolonged to this indication. Anterior plates have been thus included in multilevel strut grafts to have the ability to add instant stability to the construct. It was hypothesized that addition of anterior plates to multilevel corpectomies would possibly increase union rates, lower graft collapse and related kyphotic deformity, cut back the necessity for postoperative immobilization, and be cost-effective by allowing early mobilization and return to work. The variety of ranges has been clearly shown to influence construct failure fee in multilevel corpectomies. Complications of Buttress Plating Multilevel Anterior Cervical Corpectomies Sasso and colleagues reported a 6% failure rate in two-level constructs (2 out of 33 patients) and 71% failure fee in three-level constructs (5 out of 7 patients). However, addition of an anterior plate has two essential biomechanical penalties. Second, biomechanical research have revealed that the addition of anterior plates to multisegmental corpectomies reverses load switch via multilevel strut-grafts during flexion and extension. Importantly, the addition of an anterior plate reversed strutgraft loading mechanics. Thus, extension of roughly 10 levels gives rise to extensive loads (> 200 N). The authors concluded that software of an anterior plate in multilevel strut grafts creates supraphysiological loading which will exacerbate graft pistoning. The addition of a posterior rigidity band combined with anterior stabilization permits for an additional improve in the stiffness of the assemble. Accordingly, Schultz and colleagues report no clinically vital construct failures in 32 patients who underwent either two- or three-level corpectomies. Moreover, anterior plates that span the whole assemble have been hypothesized to stop graft settling because the Kim et al. As in most cases of multilevel corpectomies graft dislodgment occurs within the caudal finish normally at C6, C7, or T1, buttress plates are typically placed on the caudal end. One of these sufferers required revision surgery, whereas the opposite patient was handled expectantly. The preliminary report focusing on using buttress plates by Vanichkachorn and colleagues was promising.
Lateral epicondyle � Lateral (and medial) epicondyles are outside the capsular ligament erectile dysfunction caused by fatigue buy viagra professional 100 mg line. Ascending department of anterior circumflex artery � Synovial membrane of shoulder joint varieties a tubular sheath across the tendon of biceps brachii where it lies within the bicipital groove of the humerus erectile dysfunction treatment operation buy 50 mg viagra professional free shipping. Note: Tendon of lengthy head of biceps is intracapsular erectile dysfunction drugs cost comparison viagra professional 100 mg discount with visa, and extrasynovial injections for erectile dysfunction side effects viagra professional 50 mg buy line, but enclosed in the synovial sheath. Subscapularis � Subscapularis muscle attaches to lesser tubercle (and not larger tubercle). Latissimus dorsi � Latissimus dorsi attaches to the floor of intertubercular sulcus. Bones of Forearm Ulna Olecranon course of, the curved projection on the back of the elbow, receives the insertion of triceps. Coronoid process is located under the trochlear notch and offers an attachment site for the brachialis. Ulnar tuberosity is present distal to the coronoid process and in addition receives the attachment of brachialis. Radial notch accommodates the pinnacle of the radius on the superior radioulnar joint. Radius Radius head is the proximal end that articulates with the capitulum of the humerus and the radial notch of the ulna (elbow joint) and is surrounded by the annular ligament. The head and neck are free from capsular attachment and may rotate freely inside the socket. Radial tuberosity is a prominence simply inferior, has the insertion of biceps brachii tendon. The distal finish articulates with the proximal row of carpal bones (scaphoid, lunate, triquetral) but excluding pisiform. Styloid Process is a projection on the distal end of the radius (1 cm distal to that of the ulna) and receives the insertion of the brachioradialis. Nutrient arteries to both ulna & radius are branches of anterior interosseus artery department of ulnar artery. Clinical Correlations � Colles fracture of the wrist is a distal radius fracture in which the distal fragment is displaced (tilted) posteriorly, producing a characteristic bump described as dinner fork deformity. Radial and ulnar styloid process come to lie in the same line (1 cm difference is lost). Radial artery lies medial to styloid means of radius � Radius articulates with carpal bones to form radiocarpal (wrist) joint. Teres major: Greater tubercle � Attachment on higher tubercle is teres minor (and not major). Joints Joints of Upper Limb Table 3: Types of joint in higher limb Joint Sternoclavicular Acromioclavicular Shoulder Elbow Superior and inferior radioulnar Joint Middle radioulnar Wrist 1st carpometacarpal Metacarpophalangeal Intercarpal and midcarpal Type Saddle Plane Ball and socket Hinge Pivot (trochoid) Type Syndesmosis Ellipsoid > Condylar Saddle (sellar) Ellipsoid > Condylar Plane Hinge 634 Interphalangeal Upper Limb Table 4: Joint Scapula Movements, corresponding muscles and their segmental innervation Movement Elevation Depression Retraction Shoulder Protraction Flexion Muscle Upper trapezius Levator scapulae Lower trapezius Middle trapezius Rhomboids Serratus anterior Anterior deltoid Pectoralis major (clavicular head) Pectoralis main (sternocostal head) Coracobrachialis Extension Posterior deltoid Infraspinatus Teres minor Teres major Latissimus dorsi Vertical abduction Vertical adduction Middle deltoid Supraspinatus Pectoralis main (Sternocostal head) Latissimus dorsi Coracobrachialis Horizontal abduction Horizontal adduction Posterior deltoid Pectoralis major (clavicular head) Pectoralis minor Anterior deltoid Medial rotation Subscapularis: Teres major Latissimus dorsi Anterior deltoid Lateral rotation Infraspinatus Teres minor Posterior deltoid Elbow Flexion Biceps brachii Brachialis Brachioradialis Extension Supination* Pronation* Triceps brachii Biceps brachii Supinator Pronator quadratus Pronator teres Innerveation Accessory n. Sternoclavicular and Acromioclavicular Joint the sternoclavicular joint has an intra-articular fibrocartilaginous disc. Fibrous capsule is strengthened by the anterior and posterior sternoclavicular, interclavicular, and costoclavicular ligaments. It allows elevation and melancholy, protraction and retraction, and circumduction of the shoulder. It is reinforced by the rotator cuff, the glenohumeral ligaments, and the coracohumeral ligaments. Other ligaments: Three glenohumeral Ligaments (superior, middle and inferior); transverse humeral ligament prolong between the greater and lesser tubercles and holds the tendon of the long head of the biceps within the intertubercular groove; coracohumeral Ligament extends from the coracoid course of to the greater tubercle; coracoacromial Ligament extends from the coracoid course of to the acromion, prevents superior displacement of humeral head; coracoclavicular Ligament extends from the coracoid course of to the clavicle and consists of the trapezoid and conoid ligaments. Arterial supply: Suprascapular, anterior and posterior humeral circumflex, and circumflex scapular arteries. Dislocation: Anterior�inferior dislocation of the humerus is the most common sort. The head of the humerus moves anterior and inferior to the coracoid strategy of the scapula and may damage the axillary nerve or axillary artery. Abduction as much as 90� happens at the shoulder joint, additional 90� to 120� happens as humerus is rotated laterally, 120� to 180� vary is added by lateral rotation of scapula. Supraspinatus initiates abduction and causes preliminary 15� of abduction; deltoid is the primary abductor from 15� to 90� of abduction, sequentially humerus is laterally rotated by the infraspinatus and teres minor muscle tissue and subsequent overhead abduction (90��180�) is carried out by the 2 muscles primarily � trapezius and serratus anterior. During abduction, trapezius and serratus anterior cause lateral rotation of scapula and glenoid cavity ultimately faces upwards. Abduction at shoulder involves rotation of clavicle at its longitudinal axis, which happens at both the sternoclavicular and the acromioclavicular joints. Pectoralis minor � Pectoralis minor is an adjunct muscle of inspiration, which stabilizes scapula by pulling it anteriorly and inferiorly. Musculotendinous cuff stabilizes shoulder joint � Both supraspinatus and deltoid are concerned all through the vary of abduction, including the initiation of the motion. It features a synovial hinge joint, consisting of the humeroradial and humeroulnar joints, that permits flexion and extension. It also consists of the proximal radioulnar (pivot) joint, throughout the frequent capsule. Radial collateral ligament extends from the lateral epicondyle to the anterior and posterior margins of the radial notch of the ulna and the annular ligament of the radius. Ulnar collateral ligament is triangular in shape having three bands - anterior, posterior, and indirect. It extends from the medial epicondyle to the coronoid and olecranon processes of ulna. Bursae: There are three olecranon bursae: Subtendinous, which is positioned between the olecranon and the triceps tendon; Intratendinous, which may be current in the tendon of triceps brachii and Subcutaneous. Bicipitoradial bursa separates the biceps tendon from, anterior a part of the radial tuberosity. Arterial provide: Anastomosis fashioned by branches of the brachial artery and recurrent branches of the radial and ulnar arteries. It is wider in girls (than men) and disappears when the forearm is flexed or pronated. Table 6: Movements and muscle involved at elbow joint Movements Muscles concerned Flexion Primary muscles: Brachialis, biceps (in supination), brachioradialis (in mid prone). Extension Triceps, Anconeus There occurs 150� of extension and flexion, and 180� of pronosupination in conjunction with the distal radioulnar joint. Clinical Correlations � Tennis elbow (lateral epicondylitis) is brought on by a chronic inflammation or irritation of the origin (tendon) of the extensor muscles of the forearm from the lateral epicondyle of the humerus as a outcome of repetitive strain. Avoidance of repetitive bending (flexing) of the forearm is advised to find a way to not compress the ulnar nerve. It is attributable to a partial tear (or loose) of the annular ligament and thus the radial head to slip out of position. In superior Radioulnar Joint head of the radius articulates with the radial notch of the ulna, rotate throughout the encircling annular ligament and take part in pronation and supination. Table 7: Radioulnar joints: Movement and muscle tissue involved Movements Pronation Supination Muscles involved Pronator quadratus (strong pronator), pronator teres (Rapid pronator), brachioradialis* Supinator (in extended elbow), Biceps (in flexed elbow), brachioradialis* *Brachioradialis pronates/supinates the forearm to midprone position. It is fashioned by articulation of the distal finish of the radius and the articular disc of the triangular fibrocartilage with the Its capsule is strengthened by radial and ulnar collateral ligaments and dorsal and palmar radiocarpal ligaments. Midcarpal Joint is current between the proximal and distal rows of carpal bones and allows gliding and sliding movements. The wrist complex allows flexion and extension of about 140�, and 70� of adduction and abduction. Condylar � the wrist (radiocarpal) joint is a ellipsoid sort of synovial joint, though some authors think about it as condylar variety. Flexor carpi ulnaris � Flexor carpi ulnaris causes flexion on the wrist joint and ulnar deviation (adduction) as properly. Flexor carpi radialis � Abduction of the hand occurs on the wrist joint, carried out by the muscles like Flexor carpi radialis. Weight Transmission Weight of the upper limb is transmitted to the axial skeleton by numerous bones, joints and ligaments. From radius the line of transmission of weight passes to the ulna through interosseous ligament (middle radioulnar joint). Scapula transmits the load of upper limb to the clavicle through the coracoclavicular ligament and acromioclavicular joint. Clavicle transmits the burden of the higher limb to the axial skeleton (rib and sternum) by way of the sternoclavicular joint and ligaments like costoclavicular ligament.
Milkweed (Canadian Hemp). Viagra Professional.
- How does Canadian Hemp work?
- Warts, heart problems, increasing urine, asthma, coughs, swelling, and syphilis.
- What is Canadian Hemp?
- Are there any interactions with medications?
- Dosing considerations for Canadian Hemp.
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96234
The taste area is situated within the inferior part of the postcentral gyrus (primary sensory cortex) erectile dysfunction tools generic viagra professional 100 mg on line. Taste sensation from the epiglottis is carried by the internal laryngeal branch of the superior laryngeal nerve (branch of the vagus) erectile dysfunction effects 50 mg viagra professional order fast delivery. It can be known as security muscle of tongue because it prevents backward fall of tongue into the oral cavity erectile dysfunction tampa buy 100 mg viagra professional with mastercard, especially if the patient is unconscious erectile dysfunction 40 year old man viagra professional 50 mg without prescription. Taste sensation from anterior 2/3rd of tongue is carried by chorda tympani (branch of facial nerve), in course of the facial nerve and geniculate ganglion. Apical vessels drain the tip and inferior surface of the tongue into submental lymph nodes after piercing the mylohyoid muscle. Their efferents go to the submandibular nodes mainly, some cross the hyoid bone to reach the jugulo-omohyoid nodes. Sulcus terminalis V shape structure which divides the tongue into anterior two-thirds (oral part) and posterior one-third (pharyngeal part). The two elements differ in their developmental origin and accordingly mucosa, innervation and lymphatic drainage as properly. Sulcus terminalis Teeth Development Teeth are derived from neural crest cells and the floor ectoderm. Neural crest cells kind the odontoblast which forms the dentin of enamel, whereas the surface ectoderm give ameloblasts, A dental lamina develops in the oral epithelium (ectoderm origin) as a downgrowth into the underlying mesenchyme the enamel organs are derived from ectoderm and develop first for the deciduous teeth, subsequent the permanent tooth, and the dental papillae are shaped by a condensation of neural crest mesenchyme that underlie the enamel organs, and provides the dental sacs are formed by a condensation of neural crest mesenchyme surrounding the dental papillae, and provides rise to cementoblasts (which type cementum) and the periodontal ligaments. The figures within the inset present formation of dental lamina (a) and tooth buds of all deciduous teeth (b) Deciduous (primary) teeth are twenty in quantity: Two incisors, one canine, and two molars in every quadrant. Permanent teeth are thirty two in number: Two incisors, one canine, two premolars, and three molars in each quadrant. Permanent enamel Permanent tooth Eruption (years) Central incisor 7�8 Lateral incisor 8�9 Canine 10�12 1st Premolar 10�11 2nd Premolar 11�12 1st Molar 6�7 2nd Molar 12 3rd Molar 13�25 Structure: Enamel is the toughest substance (in our body) that covers the crown. It incorporates numerous blood vessels, nerves, and Parts of the Teeth: the Crown projects above the gingival surface and is covered by enamel, neck is the constricted space at lymphatics, which enter the pulp through an apical foramen at the apex of the foundation. Each maxillary molar usually has three roots, and every mandibular molar has two roots. Types of Teeth: Incisors are chisel-shaped enamel used for slicing or biting, have a single root. The higher first premolar tooth may be bifid, and all others each have a single root. Molars, which usually have three (sometimes three to five) cusps, are used for grinding. Nerve supply of Teeth and Gums Maxillary Teeth are innervated by the anterior, center, and posterior, superior alveolar branches of the maxillary nerve. Mandibular Teeth are supplied by the inferior alveolar department of the mandibular nerve. In maxillary Gingiva the outer (buccal) surface is innervated by posterior, center, and anterior superior alveolar and infraorbital nerves. In mandibular Gingiva the buccal floor is innervated by buccal and psychological nerves. Tooth pulp � the dental papillae are shaped by a condensation of neural crest mesenchyme that underlie the enamel organs, and provides rise to the odontoblasts (which type dentin) and dental pulp. Enamel is fashioned by ameloblast cells developing in surface ectoderm of oral cavity. The dental papillae are formed by a condensation of neural crest mesenchyme that underlie the enamel organs, and give rise to the odontoblasts (which form dentin) and dental pulp. Middle superior alveolar nerve is a branch of the infraorbital nerve (branch of maxillary nerve), to provide the upper premolars. Maxillary nerve � Salivary Glands Development Salivary glands develop in the oral epithelium. Submandibular and sublingual glands also develop from surface ectoderm lining the oral cavity, although some authors consider these two glands develop each from ectoderm and endoderm. Parotid Gland Parotid gland is the biggest of the three salivary glands and occupies the retromandibular house between the ramus of the mandible in front and the mastoid process and the sternocleidomastoid muscle behind. It is invested with a dense fibrous capsule, the parotid sheath, derived from the investing layer of the deep cervical fascia. It is separated from the submandibular gland by a facial extension and the stylomandibular ligament, which extends from the styloid course of to the angle of the mandible. Mastoid course of lined by two muscular tissues (sternocleidomastoid laterally and posterior stomach of digastric muscle medially). Styloid process lined by three muscle tissue (styloglossus, stylopharyngeus, and stylohyoid). Relations of parotid gland Anteromedial Surface is deeply grooved by the posterior border of the ramus of the mandible with covering muscular tissues and lateral facet of the temporomandibular joint. Postero medial surface is moulded onto the mastoid and styloid processes and their overlaying muscles. The styloid course of separate the gland from inner carotid artery, inner jugular vein, and final four cranial nerves. Superficial Surface covered from superficial to deep by pores and skin, superficial fascia containing anterior branches of higher auricular nerve, superficial parotid (preauricular) lymph nodes, platysma, parotid fascia and deeper parotid lymph nodes. Also observe the constructions pierced by it throughout its course from the parotid gland to the vestibule of the mouth Parotid gland secretes copious watery (serous) saliva by parasympathetic stimulation and produces a small quantity of the parasympathetic (secretomotor) innervation pathway is: Inferior salivatory nucleus glossopharyngeal nerve viscous saliva by sympathetic stimulation. Otic Ganglion lies in the infratemporal fossa, just below the foramen ovale between the mandibular nerve and the tensor veli palatini (muscle is deeper and medial). Preganglionic axons originate within the inferior salivatory nucleus and travel in the glossopharyngeal nerve and its tympanic department. Postganglionic fibres pass by communicating branches to the auriculotemporal nerve, which conveys them to the parotid gland. Stimulation of the lesser petrosal nerve produces vasodilator and secretomotor effects. Head and Neck � the auriculotemporal nerve accommodates parasympathetic cholinergic (secretomotor), sensory, and sympathetic fibres. A stimulus intended for salivation evokes cutaneous hyperesthesia, sweating, and flushing. It can happen after parotid surgery and could additionally be handled by chopping the tympanic plexus within the middle ear. Denervation by tympanic neurectomy or auriculotemporal nerve avulsion may be advocated, however are often not healing. The signs may be managed by the subcutaneous infiltration of purified botulinum toxin into the affected area, and use of antiperspirant. Anterior to middle meningeal artery Lateral to tensor veli palatini Lateral to mandibular nerve Inferior to foramen ovale four. After removing of the parotid gland, patient is having sweating on cheeks while eating. Auriculotemporal nerve which incorporates parasympathetic secretomotor fibers to parotid gland have reinnervated which nerve Tympanic nerve � Inferior salivatory nucleus sends preganglionic parasympathetic fibres through tympanic branch of glossopharyngeal nerve, which varieties tympanic plexus in the center ear cavity, and sends fibres by way of lesser petrosal nerve to reach the otic ganglion. Parasympathetic secretomotor fibres to the parotid gland are carried by the lesser petrosal and never the larger petrosal nerve. Greater petrosal nerve carries secretomotor fibres to the pterygopalatine ganglion and provides the lacrimal, nasal and palatine glands. Secretory fibres to the parotid gland begin in the inferior salivatory nucleus (brainstem) glossopharyngeal nerve tympanic branch tympanic plexus lesser petrosal nerve otic ganglion auriculotemporal nerve parotid gland. Tympanic plexus is current within the middle ear and receives the preganglionic fibres from the glossopharyngeal nerve. Otic ganglion lies simply inferior to the foramen ovale, via which the lesser petrosal nerve passes and carries the preganglionic fibres to the ganglion. Auriculotemporal nerve is a branch of mandibular nerve, which carries the postganglionic fibres from the otic ganglion to the parotid gland. Buccal � � � � � � � this can be a case of post-parotidectomy gustatory sweating, resulting in sweating on the cheek (buccal nerve territory).
It lies in entrance of the center 4 thoracic vertebrae (T5�T8) within the lying-down position and descends one vertebra within the erect posture (T6�T9) erectile dysfunction treatment phoenix discount 50 mg viagra professional fast delivery. The base is separated from vertebral column by the indirect pericardial sinus erectile dysfunction pump amazon discount viagra professional 50 mg with visa, esophagus erectile dysfunction treatment wikipedia order 100 mg viagra professional with amex, and aorta erectile dysfunction age graph viagra professional 50 mg discount line. Some authors contemplate the bottom of the center because the higher border of the guts where great blood vessels (superior vena cava, ascending aorta and pulmonary trunk) are hooked up. Cardiac apex is the blunt rounded extremity of the center fashioned by the left ventricle, which is directed anteroinferiorly and to the left. The apex is located mostly behind the fifth left intercostal house, near or somewhat medial to the midclavicular line. It is formed primarily by the left ventricle (2/3) and partly right ventricle (1/3) that are separated from one another by the posterior interventricular groove. Left surface is shaped primarily by the left ventricle and partly by the left atrium and auricle. The wall of the guts consists of three layers: inner endocardium, middle myocardium, and outer epicardium. Grooves/sulci Coronary (atrioventricular) sulcus is current on the exterior surface of the guts, in a circumferential manner across the heart, marks the division between the atria and the ventricles. The crux is the purpose at which the interventricular and interatrial sulci cross the coronary sulcus. Left half of anterior half is small and lodges circumflex department of left coronary artery. Base of the center is the posterior surface of heart and extends from T 5 to T eight thoracic vertebra ranges in supine posture. Left and right atrium Base of the center is the posterior floor of heart and is mainly contributed by left atrium and partly proper atrium. Diaphragmatic surface of coronary heart is majorly contributed by left ventricle and partly proper ventricle. Contains left anterior descending coronary artery Atrioventricular groove (coronary sulcus) separates atria from ventricles. Right coronary artery lodges in right part of coronary sulcus and left coronary artery offers circumflex branch in left part of coronary sulcus. Left anterior descending coronary artery runs within the anterior interventricular groove. Heart Chambers Right atrium has an anterior rough-walled portion (atrium correct and the auricle) lined with pectinate muscles and a posteriorly located smooth-walled (sinus venarum) into which the 2 venae cavae open. Sulcus terminalis is a groove on the exterior floor of the best atrium (embryologic junction of the sinus venosus and primitive atrium) corresponding to crista terminalis on inner floor. Pectinate muscle tissue are the prominent ridges of atrial myocardium located within the interior of both auricles and the best atrium. The interior of minimi) auricle presents reticular sponge-like network of the muscular ridges 608 Thorax Right atrium is larger but thinner than the left atrium. Right auricle is the conical muscular pouch of the higher anterior portion of the best atrium, it covers the proximal part of the best coronary artery. Fossa ovalis is an oval-shaped depression in the interatrial septum and represents the location of the foramen ovale, through which blood runs from the proper atrium to the left atrium in fetal circulation. Four valveless pulmonary veins from lungs (oxygenated blood) open into the left atrium. Right ventricle is largely evident anteriorly and contributes to the most important portion of the sternocostal surface of the heart. Trabeculae carneae are irregular anastomosing muscular ridges, which type the trabeculated part of the ventricles (inflow tract) and develop embryologically from the primitive ventricle. Supraventricular crest (a C-shaped internal muscular ridge), marks the junction between the trabeculated half and smooth part of the right ventricle. Papillary muscle tissue are cone-shaped muscle tissue enveloped by endocardium, lengthen from the anterior and posterior ventricular partitions and the septum, and their apices are attached to the chordae tendineae. These contract to tighten the chordae tendineae, stopping the cusps of the tricuspid valve from being everted into the atrium, preventing regurgitation of ventricular blood into the proper atrium. Chordae tendineae extend from one papillary muscle to a couple of cusp of the tricuspid valve. It is identified as the moderator band for its ability to prevent overdistention of the ventricle and carries the right limb (Purkinje fibers) of the atrioventricular bundle from the septum to the sternocostal wall of the ventricle. Table 29: Differences of inflowing and outflowing elements of the proper ventricle Inflowing decrease half It develops from primitive ventricle It is giant in size and lies beneath the supraventricular crest Outflowing upper half It develops from bulbus cordis It is small in size and lies above the supraventricular crest It is rough because of presence of the muscular ridges-the trabeculae It is clean and types upper 1 inch conical a half of the proper ventricular carneae. It forms many of the proper ventricular chamber chamber-the infundibulum, which provides rise to pulmonary trunk Left ventricle is mainly evident at the posterior view of the center, its apex is directed downward, forward, and in the direction of the left. Crista terminalis divides proper atrium into easy posterior half and tough anterior half. Superior vena cava Inferior vena cava opening is guarded by eustachian valve (rudimentary), coronary sinus by Thebesian valve and atrioventricular opening by tricuspid valve. Aortic sinus bulging into right atrium Torus aorticus (aortic mound) is the outstanding area of the proper atrial septum, which marks the projection of the noncoronary aortic sinus into the proper atrial wall. Because the esophagus is so close to the upper chambers of the heart, clear images of those heart buildings and valves can be obtained. Valves Heart valves are located around the fibrous rings of the cardiac skeleton and are lined with endocardium. They incorporate leaflets or cusps, which shut together to seal and forestall backflow. There are two pairs of valves in the coronary heart: (a) a pair of atrioventricular valves, and (b) a pair of semilunar valves. Pulmonary valve is the semilunar valve that lies between the right ventricle and the pulmonary artery and has three cusps (anterior, right, and left). It is opened by ventricular systole and shut barely after closure of the aortic valve. Aortic valve is the semilunar valve located between the left ventricle and the aorta and is composed of three cusps (posterior, proper, and left). Its closure at the beginning of ventricular diastole causes the second (dup) heart sound. Tricuspid valve lies between the right atrium and ventricle, has anterior, posterior, and septal cusps, which are hooked up by the chordae tendineae to three papillary muscles that maintain the valve closed. It is closed through the ventricular systole, the closure contributes to the first (lubb) coronary heart sound. Mitral valve lies between the left atrium and ventricle, has two cusps: a bigger anterior and a smaller posterior both of that are tethered to papillary muscular tissues (anterolateral and posteromedial) by chordae tendineae. It is closed barely before the tricuspid valve by the ventricular contraction the closure contributes to the first (lubb) heart sound. First (lubb) heart sounds is attributable to the closure of the mitral and tricuspid valves (M1T1) at the onset of ventricular systole. Second (dup) heart sound is brought on by the closure of the aortic and pulmonary valves (A2P2) on the onset of ventricular diastole. Conduction System Conduction system of the guts is constituted by the specialised cardiac muscle cells that lie immediately beneath the endocardium and carry impulses throughout the cardiac muscle, signaling the guts chambers to contract in the proper sequence. Embryologically it develops at the upper end of crista terminalis (junction between the sinus venosus and the atrium proper). It is crescent-shaped sub-epicardial tissue (having specialised myocardial fibers) with a head, body and tail. It initiates the cardiac impulse, just because it generates impulses slightly faster than the other areas with pacemaker potential. Its pace maker perform is decided by its low maximum diastolic membrane potential and steep part four spontaneous depolarization. Atrioventricular node is an oblique, half-oval atrial construction, positioned within the best side (atrial component) of the muscular atrioventricular septum close to the ostium of the coronary sinus. Triangle of Koch: A roughly triangular space on the septal wall of the right atrium, bounded by the septal leaflet of the tricuspid valve inferiorly, the anteromedial margin of the orifice of the coronary sinus as a base, and the tendon of Todaro superiorly. It splits into right and left branches, which descend into the muscular part of the interventricular septum.